Situs inversus totalis is a rare anatomic anomaly in which the normal arrangement of the heart and viscera is reversed to form a mirror picture of their usual anatomic position. It typically poses a diagnostic dilemma during the initial assessment acute thoracoabdominal trauma.
A case is presented of the findings found on the focused assessment with sonography in trauma (FAST) examination of a young adult with situs inversus who sustained solid organ injury from blunt trauma.
Patients with situs inversus can be a challenge to physicians both diagnostically and therapeutically as these patients may have nontraditional signs and symptoms upon presentation. Expedient diagnosis of solid organ injury in these patients is important, since treatment may be affected according to which organ is injured.
Ultrasound, FAST examination, Splenic injury, Splenic hematoma, Splenic contusion, Situs inversus
Situs inversus totalis is a rare anatomic anomaly. The estimated prevalence of situs inversus varies among different populations but is generally (< 1 in 10,000 people, with a range of 1:5,000 to 1:20,000) and [1-3]. Situs inversum viscerum is that condition in which the normal arrangement of the viscera is reversed to form a mirror picture of their usual anatomic position. Visceral situs inversus can occur with or without dextrocardia. If the heart is located in the right side of the thorax, it is known as situs inversus totalis [4]. If the heart remains in the normal left side of the thorax, a much rarer condition, it is known as situs inversus with levocardia or situs inversus incompletu [5]. Situs inversus results from abnormal rotation of the primitive cardiac tube during embryogenesis of unknown mechanism and may complicate diagnosis and management of acute abdominal trauma. Patients with undiagnosed situs inversus can be a challenge to physicians both diagnostically and therapeutically as these patients may have nontraditional signs and symptoms upon presentation. We present the case of a young adult with situs inversus who sustained solid organ injury from blunt trauma and review the findings of the focused assessment with sonography in trauma (FAST) examination in this patient.
A 24-year-old male was a restrained driver in an automobile accident. He had a frontal impact at 65 mph and the air bag did release. The emergency medical services (EMS) immobilized him in a cervical collar and long spine board. He was transported to the emergency department. He complained of chest and abdominal pain. His past medical history included situs inversus totalis. He took no medications and was allergic to sulfa medications. He denied alcohol or illicit drug use and did not smoke.
He had a temperature of 36.8 ℃, blood pressure of 96/68 mmHg, heart rate of 89/minute, and a respiratory rate of 16/minute. He was in mild distress. His head examination was normal. His neck examination revealed no tenderness of deformities. He had a contusion over his right chest from the seat belt with no deformity or crepitus (Figure 1). His lung sounds were normal. His heart sounds were on the right side, but normal. His abdominal examination revealed tenderness over the left upper quadrant with guarding. His extremities and neurologic examination were normal.
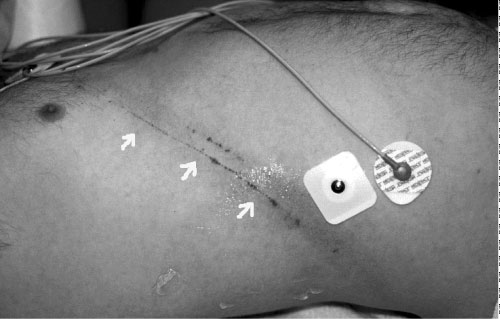 Figure 1: Contusion over the right chest from the seat belt (arrows). View Figure 1
Figure 1: Contusion over the right chest from the seat belt (arrows). View Figure 1
His white blood cell (CBC) count was 18,600/mm3, hemoglobin 16.2 g/dl, hematocrit 46.6% and platelet 192,000/mm3. His comprehensive metabolic profile, cardiac enzymes, prothrombin time (PT), and activated thromboplastin time (aPTT) were normal.
His chest radiograph demonstrated r right sided cardiac apex. His focused assessment with sonography in trauma (FAST) examination revealed the presence of fluid in Morison's pouch in the left upper quadrant (Figure 2), contusion over the spleen in the right upper side (Figure 3), but no free fluid in the pelvis or pericardial fluid. His computed tomography scan (CT) demonstrated fluid around the liver without solid liver organ injury and multiple splenic contusions (Figure 4).
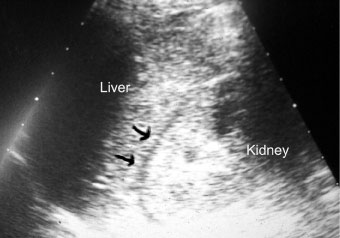 Figure 2: FAST examination shows fluid in Morison's pouch (arrows). View Figure 2
Figure 2: FAST examination shows fluid in Morison's pouch (arrows). View Figure 2
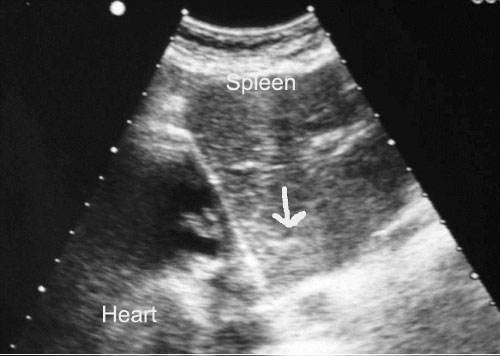 Figure 3: FAST examination shows hyperechoic areas on the spleen from a contusion (arrow). View Figure 3
Figure 3: FAST examination shows hyperechoic areas on the spleen from a contusion (arrow). View Figure 3
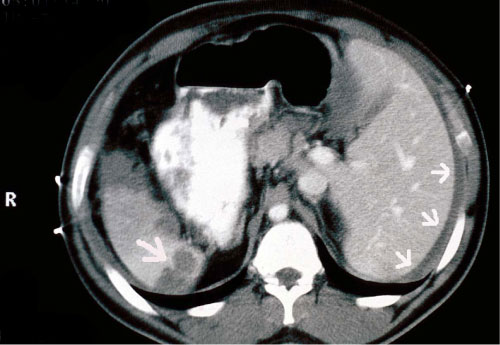 Figure 4: CT scan show perihepatic fluid (arrows on the right) and splenic contusion (arrow on the left). View Figure 4
Figure 4: CT scan show perihepatic fluid (arrows on the right) and splenic contusion (arrow on the left). View Figure 4
The patient was hospitalized and observed. He did well and was release 2 days later with no complications. He was seen in clinic 2 weeks later with no additional symptoms or complications.
Dextrocardia (the heart being located on the right side of the thorax) was first seen and drawn by Leonardo da Vinci in 1452-1519. Hieronymus Fabricius ab Aquapendente is credited with describing situs inversus in the 1606, while Marco Severino described dextrocardia in 1643 [6,7]. Situs inversus is associated with a number of other conditions, such primary ciliary dyskinesia, also known as Kartagener's (sinusitis, bronchiectasis, and situs inversus) and multiple congenital heart disorders, especially transposition of the great arteries (TGA), atrial septal defect (ASD), ventricular septal defect (VSD), pulmonary valve stenosis, patent ductus arteriosus (PDA) and tetralogy of Fallot (TOF) [8,9].
Situs denotes the position of the cardiac atria and viscera [10]. Situs solitus is the normal position, while situs inversus is the mirror image of situs solitus. Situs inversus can be classified further into situs inversus with levocardia or situs inversus with dextrocardia. In levocardia, the base-to-apex axis points to the left, and in dextrocardia, the axis is reversed. When situs cannot be determined, the patient is said to have situs ambiguous or heterotaxy. In these patients, the liver may be positioned in the midline, the spleen may be absent or may have multiple splenic tissue, the atrial morphology may be unclear, and the bowel may be malrotated. Often, structures that are normally unilateral are either duplicated or absent. Situs ambiguous tends toward symmetric morphology of normally asymmetric structures, termed isomerism. Two variants seen with situs ambiguous are asplenia syndrome and polysplenia syndrome. The asplenia syndrome is characterized by bilateral right-sidedness (right isomerism), whereas bilateral left-sidedness (left isomerism) is the hallmark of polysplenia syndrome.
Situs inversus is associated more commonly with dextrocardia [8]. A 3% to 5% incidence of congenital heart disease is observed in situs inversus with dextrocardia, particularly with transposition of the great vessels [8,9]. Of these patients, 80% have a right-sided aortic arch. Situs inversus with levocardia is rare, and it is almost always associated with congenital heart disease [5].
Situs abnormalities may be recognized first by using plain radiography or ultrasonography [2,11-14]. In most patients with situs inversus, chest radiography shows dextrocardia, with the cardiac apex pointing to the right and the aortic arch and stomach bubble located on the right as well. Ultrasound easily displays the location of the liver in the left upper quadrant and that the spleen is in the right upper quadrant [15]. Trauma in patients with situs inversus has only rarely been reported [16-23]. To our knowledge there are no case reports of the FAST examination with situs inversus. However, computed tomography (CT) scanning is the preferred examination for the definitive diagnosis of situs inversus with dextrocardia. CT scanning provides great anatomic detail for confirming visceral organ position, cardiac apical position, and great vessel branching. Magnetic resonance imaging (MRI) is usually reserved for difficult cases, where radiation exposure is a concern or for patients with associated complex cardiac anomalies [24]. This imaging modality is particularly helpful in diagnosing atrial situs and in clarifying the morphology of complex congenital heart diseases.
Surgical management in situs inversus totalis is difficult because of the altered anatomy. Anesthetic complications may arise in these patients because of the high incidence of congenital heart diseases.
Situs inversus is a rare anomaly and when confronted with a patient with trauma, their diagnosis may be confounded since location of symptoms may be atypical due to the anatomic abnormality. Expedient diagnosis of solid organ injury in these patients is important, since treatment may be affected according to which organ is injured.