Consolidation brachytherapy is a critical treatment component for locally advanced cervical cancer. The use of alternatives (linac based stereotactic radiosurgery (SRS) or external beam (EBRT) boosts) on linacs compromise oncologic results in cervical cancer patients. Our patient, a 32-year old woman with a 5 cm FIGO IIB cervical cancer, had a uterus Didelphys and was therefore not suitable for intracervical brachytherapy. Instead, she received a brachytherapy emulating robotic radiosurgery boost using CyberKnife®. 3 months after treatment she had a complete radiologic and pathologic response.
Intracervical brachytherapy remains an integral part of definitive chemoradiation in cervical cancer patients. It offers the possibility to cover the macroscopic tumor with very high doses (biologically equivalent doses of EQD2 ≥ 80 Gy.), which cannot be achieved with external beam radiation therapy techniques. There is a clear dose response relationship in terms of oncological results and toxicity [1,2].
Linac-based stereotactic radiosurgery is not considered a suitable alternative to intracervical brachytherapy because the doses prescribed are usually below the recommended EQD2 of at least 80 Gy. Benchmark parameters were defined, including EQD2 =/> 80 Gy, concomitant use of cisplatinum, implementation of brachytherapy for curative chemotherapy, treatment of at least 28 patients with primary chemo-radiation in specialized centers and an appropriate treatment time of no more than 8 weeks total treatment time [3-7].
There are some clinical situations where brachytherapy cannot be used: patients’ rejection of brachytherapy, inability to define cervix for brachytherapy applicators, presence of poorly responding or asymmetric tumors or the so-called uterus didelphys (bicornis and bicollis) where satisfactory target coverage cannot be achieved with brachytherapy. For these patients, the role of robotic radiosurgery (CyberKnife®) in brachytherapy emulation was investigated in a phase II study (Long term Results of Robotic radiosurgery for brachytherapy emulation in patients with cervical cancer, paper in preparation). The aim of the study was to evaluate the feasibility, local control and survival of patients with brachytherapy like dose prescriptions with the use of robotic radiosurgery using CyberKnife®. There already exists data on stereotactic radiation as an alternative for brachytherapy, but no outcome data is available from phase II or III studies in which brachytherapy emulation with stereotactic techniques has been systematically analyzed in the primary situation [8-16].
In this case report, we report about a patient who presented with a large FIGO IIB cervical cancer and an uterus didelphys. She was treated with primary chemoradiation using CyberKnife®.
A 32-year-old woman with severe vaginal bleeding was brought to hospital as an emergency. The gynecological examination revealed a large, exophytically growing tumor with questionable parametric infiltration. Sonographically, an approx. 35 × 55 mm large tumor was found, starting from the cervix.
A cervical carcinoma was suspected and the tumor biopsied. After vaginal tamponade there was no further bleeding.
Tumor markers were CA 125 10 kU/l (standard value < 35 kU/l), CEA 1.64 ug/l (standard value < 5.0 ug/l), SCC 21 ug/l (standard value < 1.9 ug/l).
An MRI of the pelvis showed a cervical carcinoma measuring a maximum of 50 mm starting from the posterior portio with infiltration of the dorsal vaginal vault and the left parametric region. MRT-morphologically there was no sign of enlarged pelvic or paraaortal lymph nodes. As anatomical peculiarity the patient had an uterus didelphys (uterus bicollis and bicornis) with complete double formation of the uterus including a duplicate cervix (see Figure 1a, Figure 1b, Figure 2a and Figure 2b).
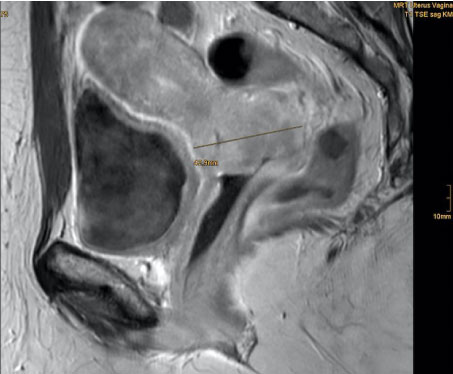 Figure 1a: T1 sequence with contrast, sagittal view. View Figure 1a
Figure 1a: T1 sequence with contrast, sagittal view. View Figure 1a
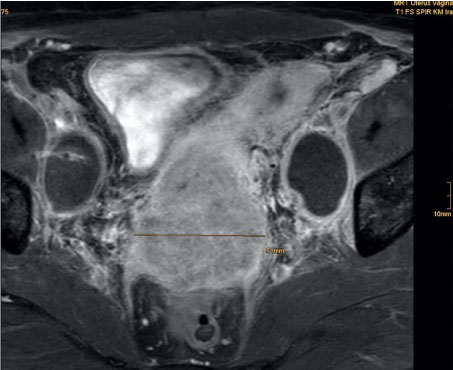 Figure 1b: T1 sequence with contrast, transversal view. View Figure 1b
Figure 1b: T1 sequence with contrast, transversal view. View Figure 1b
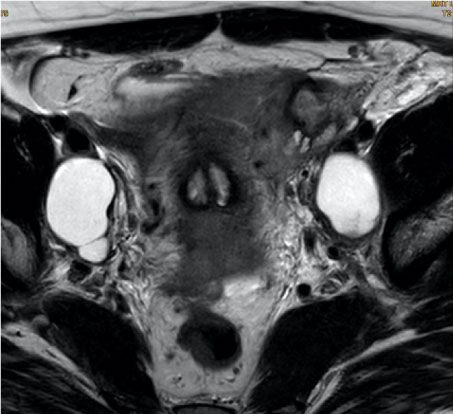 Figure 2a: Uterus didelphys (bicollis and bicornis) on MRI with double cervix. View Figure 2a
Figure 2a: Uterus didelphys (bicollis and bicornis) on MRI with double cervix. View Figure 2a
 Figure 2b: Uterus didelphys (bicollis and bicornis) on MRI with double uterus. View Figure 2b
Figure 2b: Uterus didelphys (bicollis and bicornis) on MRI with double uterus. View Figure 2b
A CT examination of the thorax and abdomen showed no evidence of thoracoabdominal metastases.
The histology of the biopsies confirmed a poorly differentiated squamous cell carcinoma with positivity for p16 as a surrogate marker for HPV infection and a proliferation index of approx. 70%.
All possible therapeutic options were discussed in the interdisciplinary tumor conference.
1.) Lymph node staging, neoadjuvant chemotherapy due to the size of the tumor, followed by radical hysterectomy and adjuvant chemoradiation of the pelvis.
2.) Lymph node staging followed by primary chemoradiation with intracervical brachytherapy.
Due to the uterus didelphys and the configuration of the tumor, the insertion of a brachytherapy applicator and the performance of intracervical after loading would not have been possible or would have been associated with severe losses in terms of dose distribution. As an alternative within the individual attempt of cure, the patient was offered brachytherapy-emulating robotic radiosurgery using the CyberKnife® system. The dose prescription is the same as for conventional brachytherapy.
The patient was informed and advised about the therapy options available to her. She decided for the individual attempt of cure using CyberKnife® boost.
In the lymph node staging, no lymph node metastasis was found in pelvic and paraaortic lymph node staging. Both ovaries were ovariopexied to the lateral pelvic wall in the same operation to maintain hormone production after radiotherapy (see Figures 3a, Figure 3b, Figure 3c, Figure 3d, Figure 3e and Figure 3f).
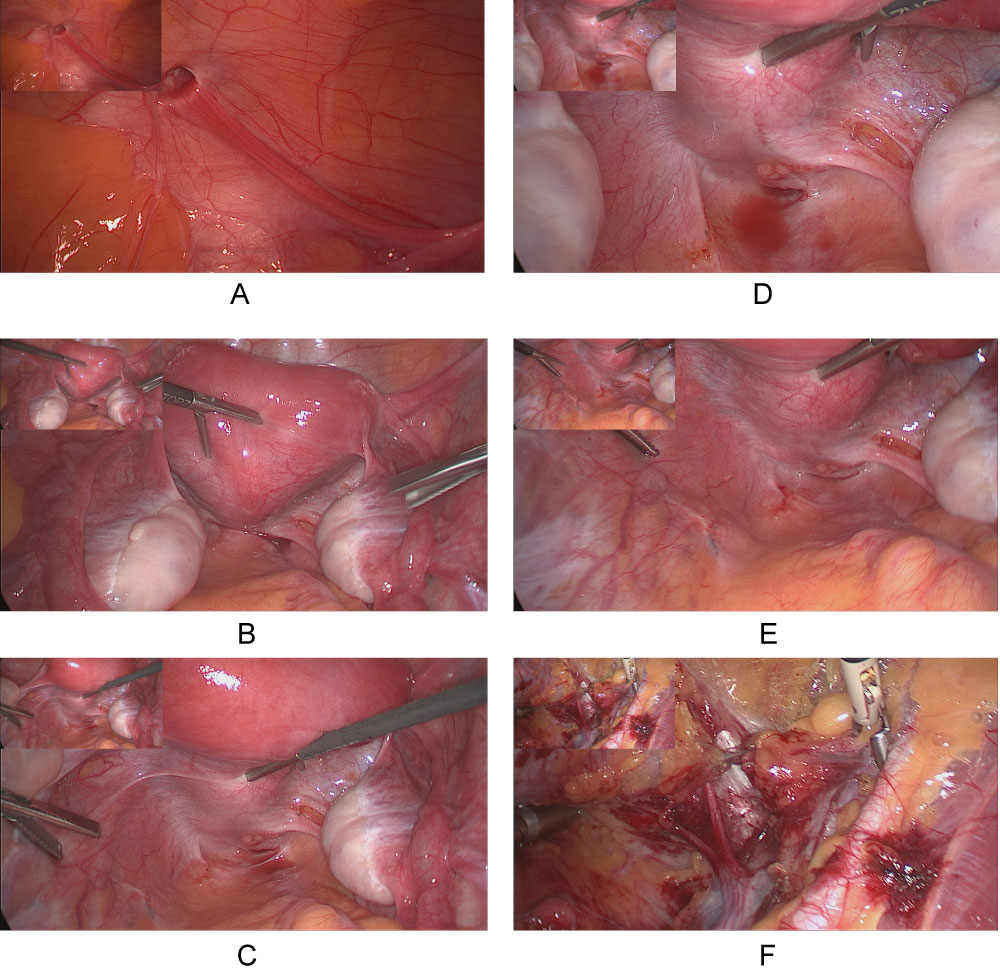 Figure 3: a-f) Laparoscopic pelvic and paraaortic lymphnode staging with ovario pexie to the lateral pelvic wall. View Figure 3
Figure 3: a-f) Laparoscopic pelvic and paraaortic lymphnode staging with ovario pexie to the lateral pelvic wall. View Figure 3
The definite tumor formula was SCC FIGO IIB pN0 (0/27) L0 V0 G3 Ki67 70% p16+.
Subsequently, the patient received primary chemoradiation. It included external beam radiation (EBRT) with 6 MV photons using volumetric arc techniques (VMAT) on a linear accelerator (Truebeam, Varian) and daily on-board images with five weekly single doses of 1.8 Gy to the primary tumor including the uterus and the pelvic lymph nodes to a total dose of 50.4 Gy in 28 fractions. A simultaneous boost was given with five weekly single doses of 2.12 Gy to both parametric regions to a total dose of 59.36 Gy in 28 fractions. Cisplatin 40 mg/m2 BSA was administered once weekly for five applications.
In the 3rd or 4th week of EBRT, a second gynecologic examination was performed and four fiducials were implanted to the right and left anterior and posterior tumor border. An additional MRI and a planning CT with an emptied rectum and emptied bladder were performed to assist target volume definition.
The non-isocentric technique of the CyberKnife® allows even complex target volumes with steep dose gradients to be irradiated precisely. The CyberKnife® boost was performed in the 4th to 6th week of treatment. Five fractions to a total dose of 25 Gy were prescribed comparable to the institutional brachytherapy concept. Two or three weekly robotic radiosurgery fractions were given (every other day) overlapping with external beam radiation (see Figure 4a and Figure 4b).
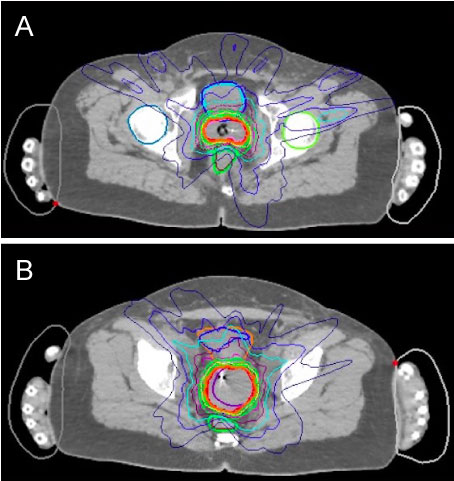 Figure 4: a,b) Dose distribution on the CyberKnife® planning software. View Figure 4
Figure 4: a,b) Dose distribution on the CyberKnife® planning software. View Figure 4
Treatment tolerability was very good. The patient suffered from mild GI and GU toxicity (grade I-II) and the usual blood count changes were observed after chemotherapy. The CyberKnife® treatment was tolerated very well without any acute toxicity.
Three months after completion of the therapy, the patient presented for the first follow up with gynecological exam, radiology and intracervical curettage. Clinically, both portios were smooth with no indication of a residual tumor. Sonographically an inconspicuous finding was documented. An intracervical curettage and an MRI were performed for control. No tumor was detected in the curettage of both cervices. MRI showed no evidence of tumor recurrence or residual tumor tissue (see Figure 4a. The hormone status was normal (LH 4.81 U/l, FSH 5.24 U/l, 17-beta-estradiol 32 ng/l, progesterone 2.06 ug/l).
Another 3 months later a new MRI control was performed without any indication of a tumor recurrence.
The patient is in excellent clinical condition and has no severe limitations due to the therapy. She suffers from a mild vaginitis.
Several other authors addressed the use of robotic radiosurgery in cervical cancer patients. Haas, et al. reported retrospectively on six consecutive patients (mean age 80 years) with anatomical or medical conditions treated with combined external beam radiation and CyberKnife® boost to the cervix. CyberKnife® was delivered with five fractions of 4 Gy single dose, one patient with received 3 × 6.5 Gy. All patients tolerated the treatment well with no grade 3 or higher urinary or rectal toxicities. Grade 1/2 urinary and bowel toxicities occurred in four patients following conventional external beam radiation. In addition, the five patients after a minimum of 12 months follow-up all (100%) remain locally and distantly controlled with no evidence of disease [9].
There is a study in preparation where a larger number of patients was treated with robotic radiosurgery as brachytherapy emulation. This study will bring us the long-term results of robotic radiosurgery in comparison with intracervical brachytherapy.
In this case study, we could demonstrate that after curettage 3-months after treatment a complete histologic response could be achieved in a situation where conventional brachytherapy would be inadequate. In contrast to linac-based boost concepts brachytherapy emulation with the CyberKnife® represents a real alternative to intracervical brachytherapy. The therapy is safe and feasible. The technique used allows excellent sparing of the organs at risk with optimum target volume coverage. The profile of side effects is favorable.
Robotic radiosurgery is a valid alternative for patients who cannot undergo intracervical brachytherapy.
The authors have no conflicts of interest.