The COVID-19 pandemic has stretched into the tiny Himalayan country Bhutan and the first suspected case was seen on 27th January 2020. There are no reports available in the country till date. Therefore, a descriptive study was conducted to understand the epidemiological characteristics of confirmed COVID-19 cases in Bhutan as of 30th April 2020.
Data were extracted from the Royal Center for Disease Control COVID-19 information database and analyzed using Epi Info 7.2.
A total of 1716 individuals were tested for SARS-CoV-2 infection and seven were confirmed positive using RT-PCR. The median age and incubation period were 20 years and 5 days respectively. The predominant clinical symptoms included loss of smell (71.0%) followed by fever (42.8%) and sore throat (42.8%). Notably, there is no reported local transmission in the country.
The robust surveillance system plays a vital role in active case findings in COVID-19 cases. Further efforts should be continually focused on surveillance and testing for the containment of the infection to prevent local transmission.
Bhutan, COVID-19, Epidemiology and surveillance
On 31st December 2019, a cluster of pneumonia cases of unknown etiology was seen linked to the seafood market of Wuhan, China [1,2]. China's Center for Disease Control (CCDC) identified the causative agent to be SARS-CoV-2, resulting in the cause of coronavirus disease (COVID-19) [3]. The World Health Organization (WHO) declared it a Public Health Emergency of International Concern (PHEIC) on 30th January 2020 [4]. The infection had rapidly affected 113 countries; thus, the event was declared pandemic on 11th March 2020. There were 3090445 confirmed cases and 217769 deaths reported globally affecting all regions as of 30th April [5].
In Bhutan, a case of COVID-19 was first suspected on 27th January. The Himalayan Kingdom of Bhutan is bordered by China to the north and India to the south and covers an area of approximately 38,394 sq.km4. In 2017, the total population of Bhutan was 735,553, making it one of the least populated countries in Asia [6].
The Royal Center for Disease Control (RCDC), being a focal point for the national disease's surveillance and outbreak investigation, enhanced its disease surveillance and prepared response to COVID-19 by mid-January. The existing influenza-like illness and severe acute respiratory illness (ILI/SARI) surveillance system was further strengthened from weekly to daily reporting. The COVID-19 database information system was also developed to monitor travelers entering the country via air and land crossing.
Currently, there are no reports available regarding the surveillance and epidemiological investigation of COVID-19 suspected cases in the country. Understanding the epidemiology of COVID-19 cases in each country is of paramount importance. This will help formulate and implement effective control strategies for the containment of the disease. Therefore, we conducted a descriptive study to understand the epidemiological characteristics of confirmed COVID-19 cases in Bhutan until 30th April 2020.
The case definition was adapted from the World Health Organization (WHO) and the Centre for Disease Control (CDC) [7]. The first case definition was developed on 21st January and updated seven times with the latest edition made on 1st April based on the evolving disease epidemiology.
To prevent community transmission, a 21-day facility quarantine measure has been implemented by the government for travelers entering Bhutan and for the primary contact of the confirmed cases [8]. They were quarantined in designated quarantine facilities across all 20 districts of the country.
Upon detection of the confirmed case, contact tracing was done for all the contacts fulfilling the definition of primary contact and were placed under designated quarantine facilities [7,9]. Their health status was monitored daily and individuals who developed symptoms were tested for SARS-CoV-2 infection.
Upper respiratory samples (nasal and throat swabs) were collected and tested for SARS-CoV-2 infection using real time reverse transcriptase polymerase chain reaction (RT-PCR) as per the standard testing protocols developed by the WHO [10].
A standard case investigation form (CIF) was used to collect socio-demographic information, clinical details, and history of exposure (travel history and contact exposure). The personal identification details were removed for analysis to maintain confidentiality. Data were retrieved from the RCDC COVID-19 information system and analyzed using Epi Info version 7.2.2.6. The incubation period was estimated based on the estimated exposure date and the date of symptom onset.
A total of 1716 individuals were tested for COVID-19 from 27th January to 30th April 2020. Of those tested, seven (0.40%) were laboratory-confirmed positive. From the positive cases, two were male and five female who were travelers. The first two cases were American tourists, while the rest were Bhutanese residing abroad.
The median age of the confirmed cases was 24 years (range: 16-76 years). The common clinical symptoms included loss of smell (71.0%), cough (42.8%), fever (42.8%), diarrhea (33.3%), and sore throat (42.8%). The median incubation period of the seven cases was 5 days (range: 4-7 days). All cases were immediately isolated in the isolation ward at Jigme Dorji Wangchuck National Referral Hospital (JDWNRH).
A 76-year-old man, an American tourist was the first confirmed COVID-19 case detected on 5th March 2020. While a 59 years female, his partner was the second case detected on 19th March.
Case 001 experienced abdominal bloating and discomfort on 28th February, while they were on a seven days cruise trip at Brahmaputra River in Assam, India. His symptoms continued after reaching Bhutan, upon which he visited the outpatient department (OPD) of the JDWNRH and received symptomatic treatment. However, his condition deteriorated, and on 5th March, he re-visited the emergency department of JDWNRH. He was then advised for the test and was tested positive for SARS-CoV-2 infection. He was admitted to the isolation ward of JDWNRH until air evacuated on 13th March.
Case 002, being a high-risk close contact was also isolated on the same night of 5th March and kept under observation. She tested negative three times on 6th, 8th and 11th March, while her fourth samples tested positive for SARS-CoV-2 infection on 19th. Based on the medium incubation period of 5-6 days [11,12], the likely source of acquiring the infection by the case 001 was from the cruise ship. The case 002 was a close contact and she was providing care to her partner (Figure 1).
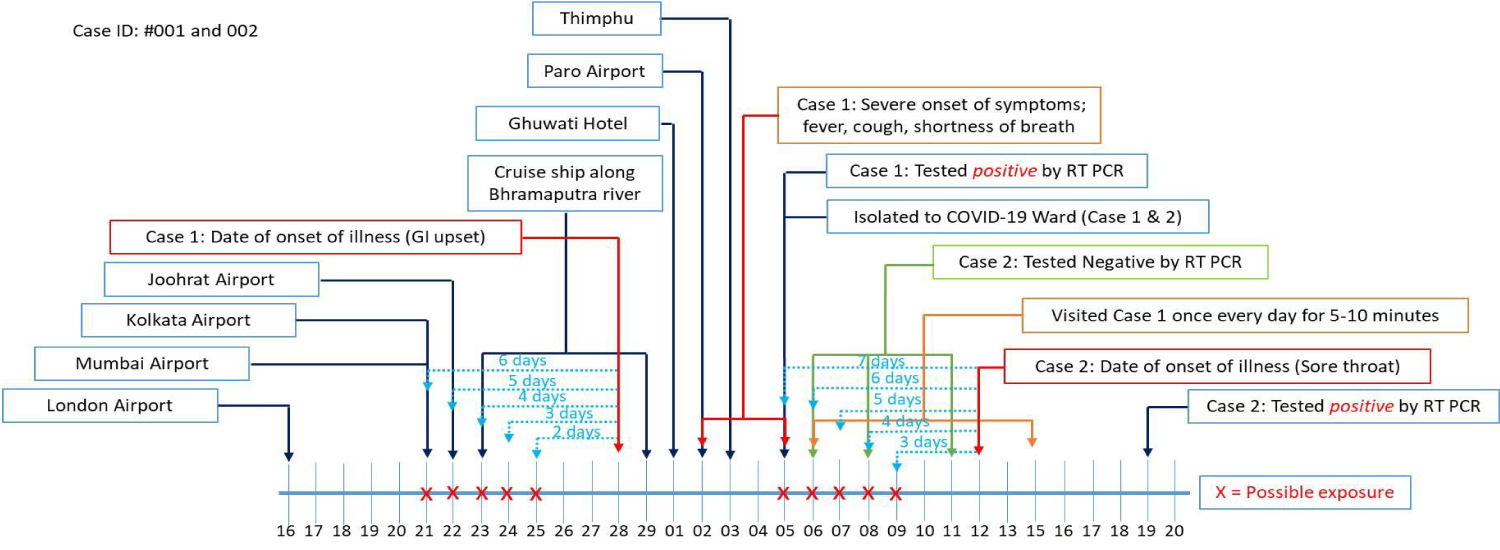 Figure 1: Timeline of travel, activities, onset of illness in Cases 001 and 002.
View Figure 1
Figure 1: Timeline of travel, activities, onset of illness in Cases 001 and 002.
View Figure 1
Case 003 was a 20-year-old female Bhutanese student in London, arrived at Paro International Airport on 22nd March (via Singapore). She complained of low-grade fever, generalized body ache and loss of appetite on 25th March, where her sample was tested and confirmed positive for SARS-CoV-2 infection. Based on the medium incubation period of 5-6 days [11,12], the likely sources of her infection were Singapore Airport (stayed transit for 18 hours) and Heathrow Airport, London/Inflight (Figure 2).
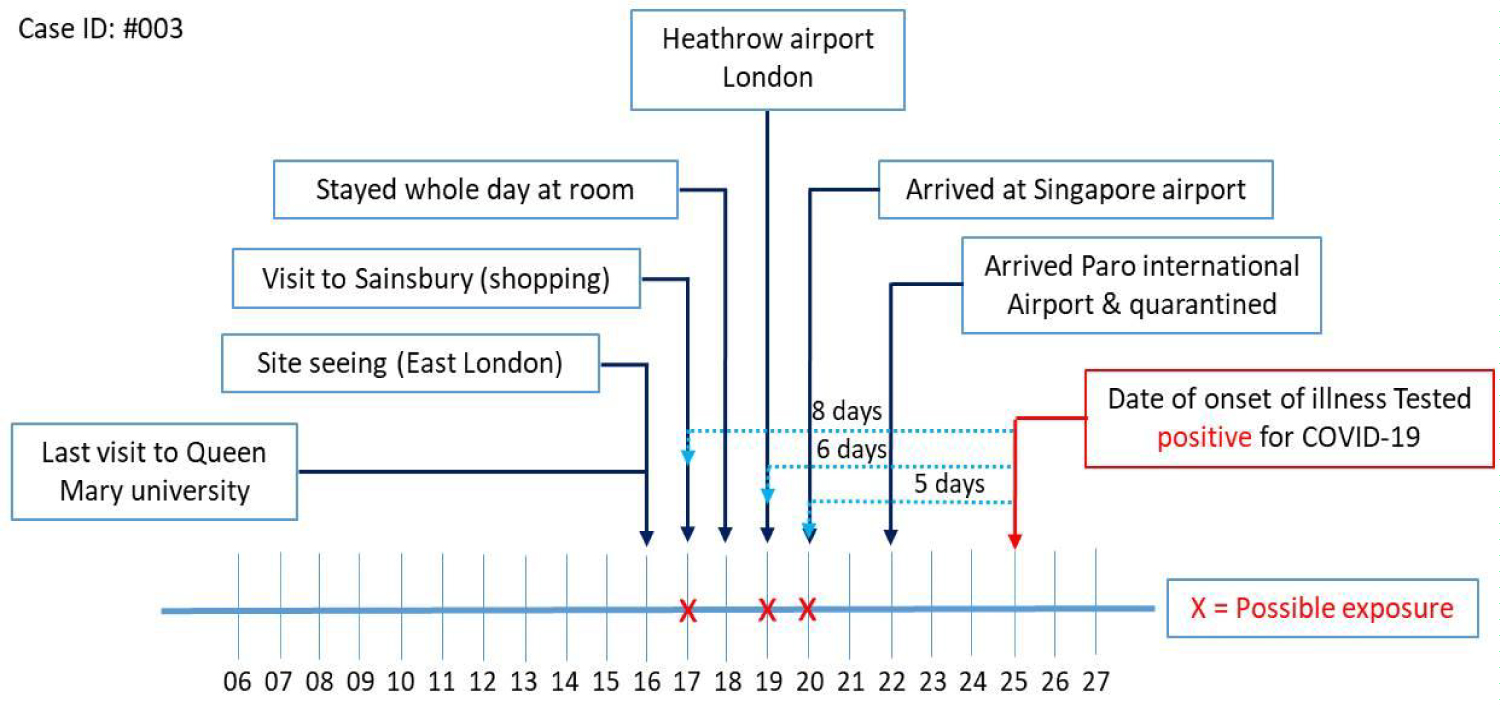 Figure 2: Timeline of travel, activities and onset of illness in Case 003.
View Figure 2
Figure 2: Timeline of travel, activities and onset of illness in Case 003.
View Figure 2
Case 004 was another 20-year-old female Bhutanese student in London, arrived at Paro International Airport on 18th March (via Delhi). She had three episodes of diarrhea on the 21st March, and later subsided. She complained of nasal congestion and loss of smell (anosmia) on the 28th March, upon which her sample was collected and tested. Based on the medium incubation period of 5-6 days [11,12], the likely sources of her infection were Heathrow airport and Sainsbury supermarket (Figure 3).
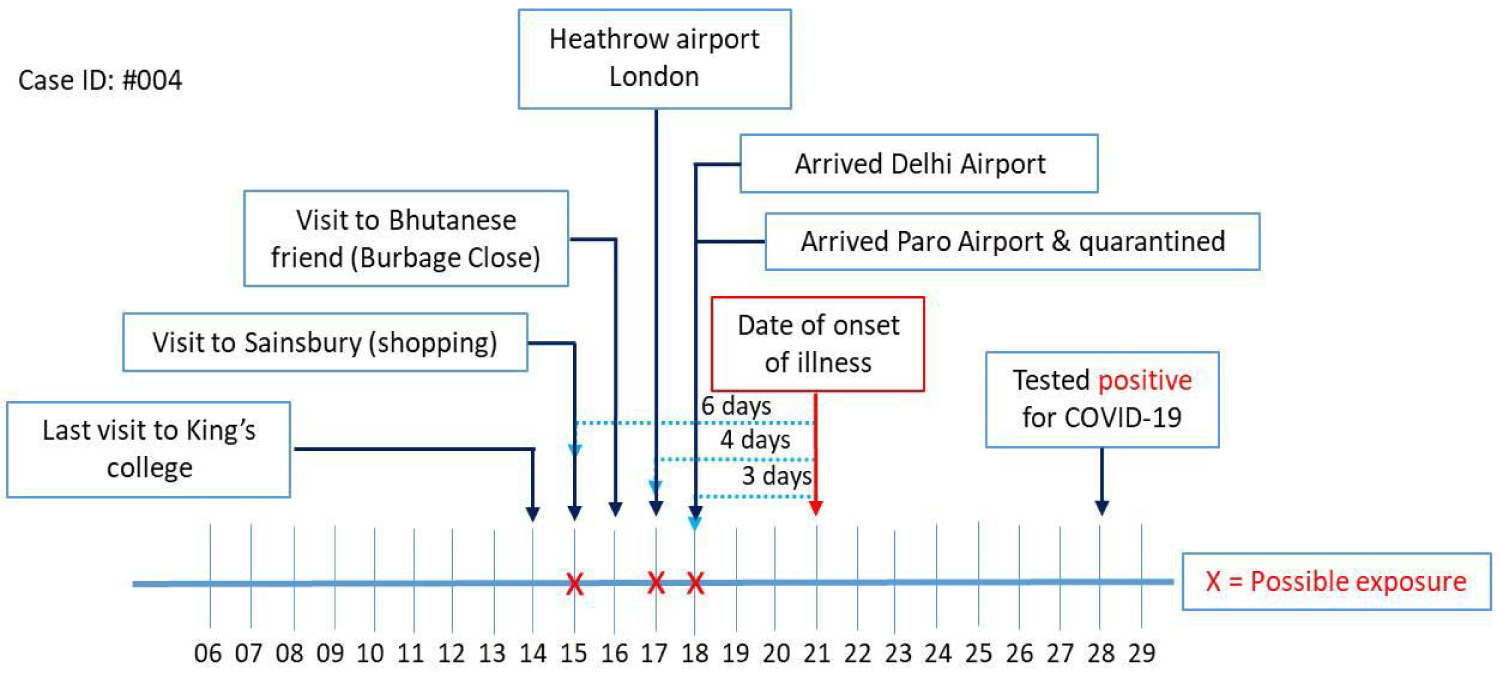 Figure 3: Timeline of travel, activities and onset of illness in case 004.
View Figure 3
Figure 3: Timeline of travel, activities and onset of illness in case 004.
View Figure 3
Case 005 was a 16-year-old female Bhutanese student in New York, United States arrived at Paro International Airport on 31st March (via Delhi, India). As a mandatory health requirement to test all travelers arriving from affected countries, her sample was collected and tested positive for COVID-19 on the same night. Based on the medium incubation period of 5-6 days [11,12], her likely source of acquiring the infection was Jackson Heights (Figure 4).
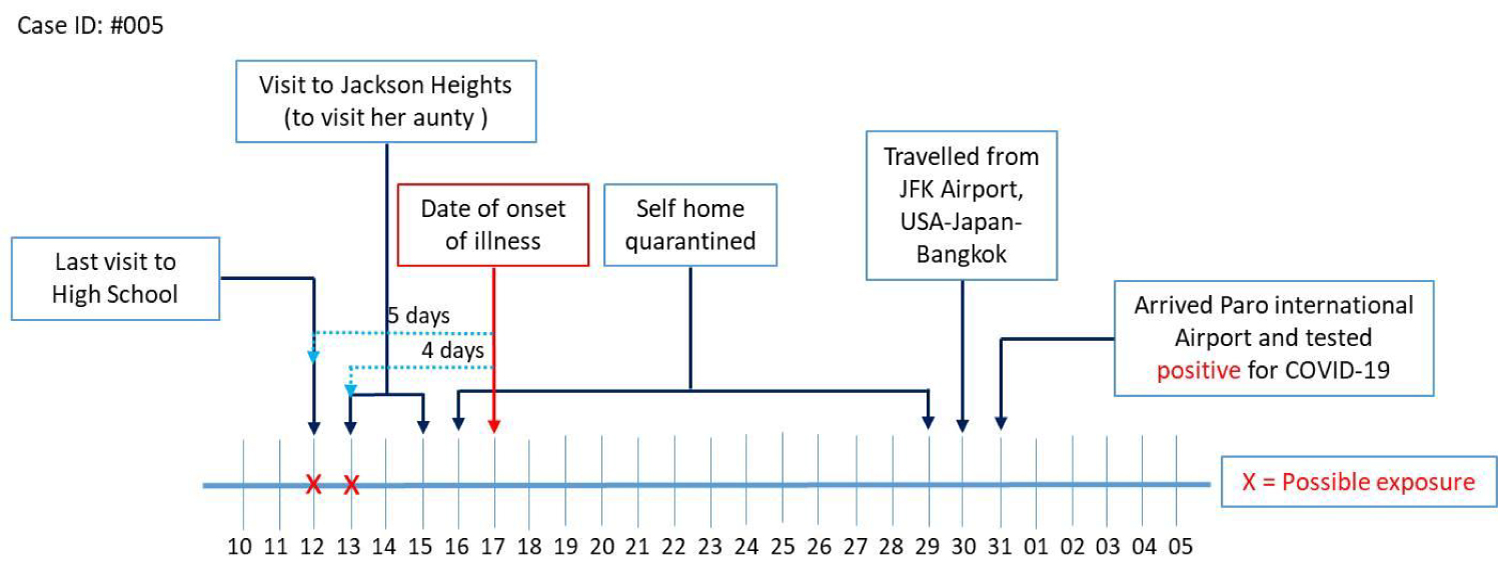 Figure 4: Timeline of travel, activities and onset of illness in Case 005.
View Figure 4
Figure 4: Timeline of travel, activities and onset of illness in Case 005.
View Figure 4
Case 006 was a 24-year-old Bhutanese female, an overseas worker in Dubai, arrived at Paro International Airport on 18th April. On the morning of 20th April, she complained of sore throat with few episodes of cough, where upon her samples were collected and tested positive for COVID-19. Based on the medium incubation period of 5-6 days [11,12], the likely source of acquiring the infection was Binsoughg mall (Figure 5).
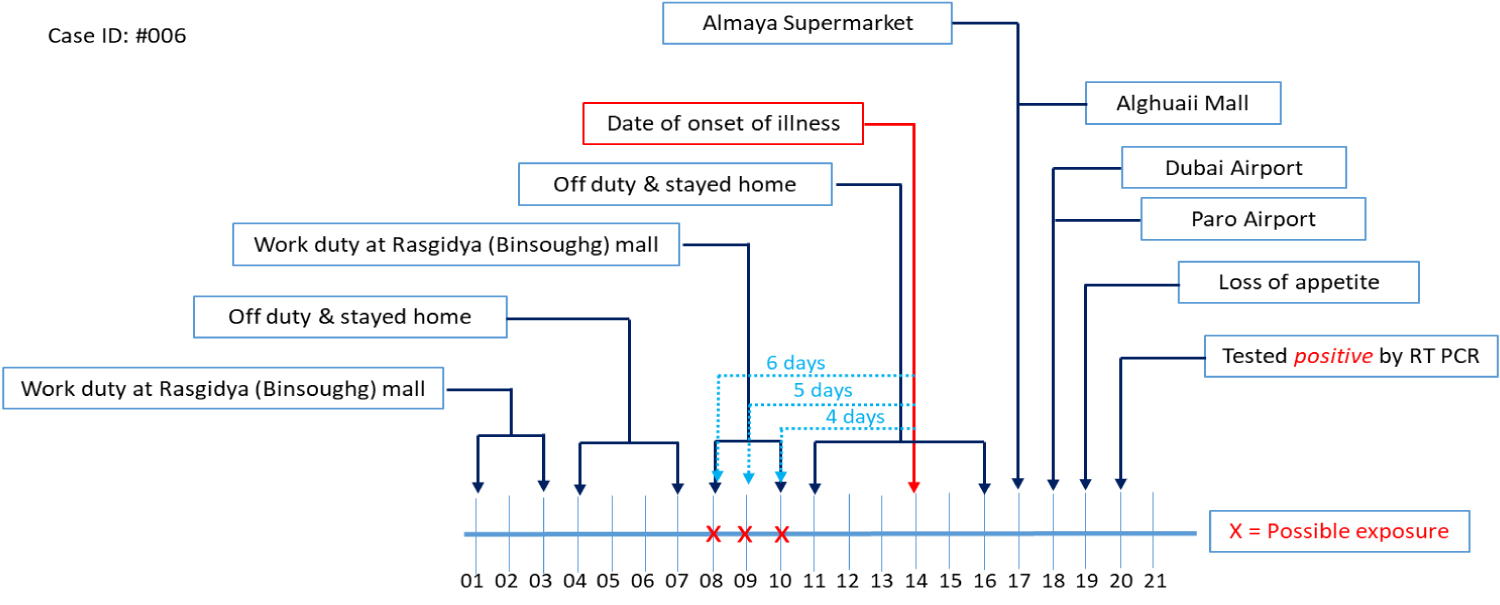 Figure 5: Timeline of travel, activities and onset of illness in Case 006.
View Figure 5
Figure 5: Timeline of travel, activities and onset of illness in Case 006.
View Figure 5
Case 007 was a 24-year-old Bhutanese male, an overseas worker in Qatar, arrived at Paro International Airport on 21st April. The sample for PCR was collected immediately on his arrival, considering the Middle East as a high-risk region. The sample was tested on 22nd April and confirmed positive for COVID-19. Based on the medium incubation period of 5-6 days [11,12], his likely sources of infection were the Wassef Office, Abu Hamour Office, Ooredoo Office, New World shopping center and Hamad Airport (Figure 6).
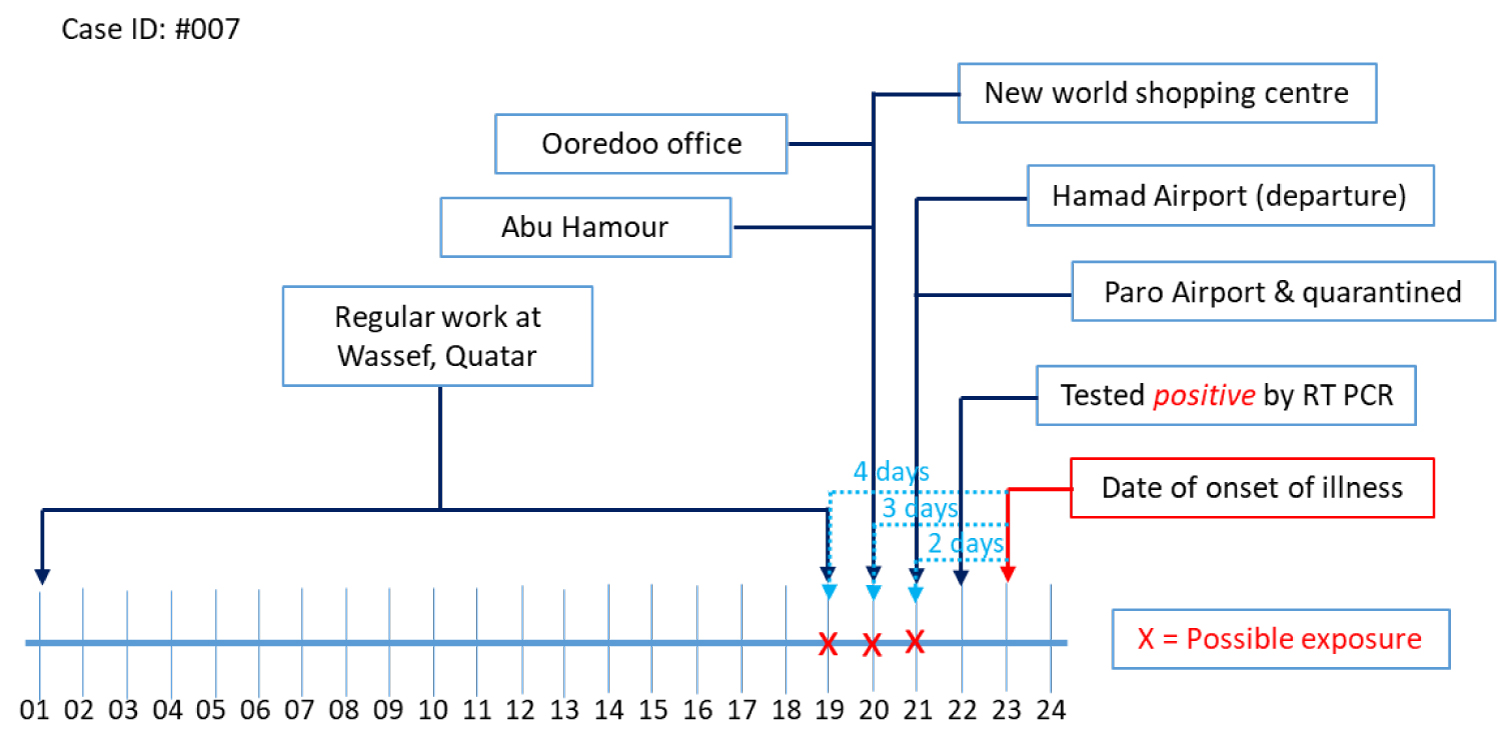 Figure 6: Timeline of travel, activities and onset of illness in Case 007.
View Figure 6
Figure 6: Timeline of travel, activities and onset of illness in Case 007.
View Figure 6
There were a total of 224 contacts that were tested for SARS-CoV-2 infection in the country from 6th March to 30th April 2020. All the contacts tested negative except for the close contact of case 001. The median age for the contacts was 29 years and there were more males (54.0%) than female (46.0%). Bhutan developed a contact tracing app called "Druk Trace" mobile app, intended for "Contact Tracing" by helping with the identification of people who may have come in direct contact with a COVID-19 infected person while visiting public places or while using public transportation. Every office, business entity, and public transport were required to publicly display a QR code generated from the app and all individuals were mandated to use the app to scan the QR code every time they enter these public places or use public transportation. Those who do not have smartphones were required to provide contact information to be filled in the log files that were to be managed by the respective offices and drivers.
All seven cases were classified as imported cases and displayed mild symptoms with no sign of severity at the time of diagnosis. Increasing evidence suggests that mild clinical symptoms could be more frequent in COVID-19 cases than in other coronavirus infections [13-15]. The common clinical symptoms in our cases include loss of smell (71.0%) and similar symptoms were also reported [16-18].
The positivity rate in our study was 0.40%, which was relatively lower compared to the reports reported in Asia and Europe [19]. This may be attributed to the aggressive surveillance system of the country and the highest testing rate in the South Asia region [20]. The country also follows the WHO strategy of Test, Test, Test, and isolate [21].
The delay in detection of case 001 would probably be due to his only complaint of GI disturbances that did not meet the case definition for laboratory testing. With zero cases detected in the country at that time, there was a low suspicion of COVID-19 by clinicians, especially when a patient presented with atypical symptoms. The typical clinical manifestations of COVID-19 was fever, cough and shortness of breath [7,22]. Studies conducted in China and the US reported that the majority of the cases are asymptomatic and only few evidence existed that COVID-19 patients exhibit gastrointestinal problems [15,23-25].
The SARS- CoV-2 virus binds to ACE receptors, which are found in the respiratory tract, GI tract and kidneys [26]. Thus, in this typical case, the virus may have entered via the GI system and later in the systemic circulation making the case intricate.
Case 002 is the close partner of the first case and was together from 21st February to 12th March. She was giving care during his illness, however, only her fourth sample came positive on 19th March. The delay in detection could be that her partner showed no respiratory symptoms from where he could transmit the virus through droplets. A study conducted in several countries reported that the chances of transmitting virus by asymptomatic cases are low compared to those with symptoms [14,15,27]. Other possibility would be the quality of the samples. A study by Patel reported that the detection of COVID-19 purely lies in the quality of samples [10,28].
All the contacts of all confirmed cases were mandatorily quarantined at designated facility for 21-days and monitored. This was attributed to the lack of not having any community transmission in the country. The reports by WHO/CDC consistently conclude that quarantine can play a role in controlling the spread of coronavirus SARS-CoV-2 [29,30]. The active surveillance of all travelers and contacts of the confirmed cases and implementation of prevention and control measures prevented the risk of human-to-human transmission originating from imported cases, which is in accordance with other reports [31,32].
The detailed clinical information of the cases was unavailable at the time of analysis. Moreover, symptom-onset dates and exposure history of cases were based on telephonic interviews, which might have overestimated or underestimated as the respondents could be influenced by potential recall bias.
Seven cases were detected positive for COVID-19 by RT-PCR, and all cases were imported. All cases displayed mild symptoms, with many young Bhutanese experiencing loss of smell and taste. The median incubation period of seven cases was 5 (range 4-7 days), and notably, no cases of local transmission had been seen till date. Further efforts should be continually focused on surveillance, testing and containment efforts such as facility quarantine, social distancing and hand hygiene to prevent community transmission. An active case finding among close contacts of cases and traveler would prevent further spread of the disease in the community.
We thank all the staff of the RCDC, the surveillance team of the Ministry of Health and the patients.
The authors declare no conflicts of interest.
There was no funding support required for this study.
KG, AM and JBD designed the study concept and design, drafted and the manuscript, analysis and interpretation of the data; SW, TD and LMA revision of the manuscript.