Surgeons require accurate ranges of normal small bowel length (SBL) to benefit patients. The relationship between cadaveric SBL and in vivo human SBL is not known. We hypothesized that cadaveric SBL is significantly different compared to human SBL.
SBL was measured prospectively in 167 formalin-fixed cadavers; and studied in 118 without intestinal surgery. A standardized and reproducible method of small bowel measurement was utilized in both in vivo and cadaveric subjects. Small bowel was measured in situ from the Ligament of Treitz to the ileocecal valve. These measurements were compared to previously published cadaveric and in vivo human SBL data. The number of cadavers examined was larger than in other published studies; the number of in vivo subjects was also the highest yet reported.
Formalin-fixed cadavers had significantly shorter SBL than living subjects- 366.1±82.7 vs 508.6±105.8 cm (mean + sd, p < 0.0001). The mean fresh cadaveric SBLs (592.8 cm) was longer in comparison to the formalin-fixed cadaver SBL (366 cm). In cadavers, univariate analysis showed that age (younger > older), height (taller > shorter), and gender (male > female) correlated with SBL (p < 0.01). In multivariate analysis, only height remained predictive of SBL (p < 0.0001). Torso length was positively correlated with SBL (cricoid to jugular notch, sternal angle, xiphoid, umbilicus, pubic tubercle), p < 0.0001 top = 0.005. Torso circumferences at the xiphoid-sternal angle, subcostal line, umbilicus, and iliac crest were all positively correlated with SBL (p = 0.005).
To date, this study remains the first to compare detailed physical measurements to SBL. In vivo SBL was significantly longer than formalin-fixed cadaver SBL. Height was a primary predictor of SBL. Cadaveric SBL measurements should not be used to estimate normative SBL data in living subjects.
Small bowel, Small intestine, Length, Measurement, Anatomy, Short bowel syndrome, Cadaver, Human, Trauma
SBL: Small Bowel Length
The small intestine encompasses the majority of digestive and absorptive properties of the gastrointestinal system. Disease processes that disrupt small bowel length (SBL) and/or function hinder human growth and metabolism [1,2]. Physical and/or functional shortening of the small bowel may result in intestinal failure (characterized by inability to maintain fluid, electrolyte, micronutrient, and protein-energy balance). For this reason, understanding accurate SBL in living subjects is crucial. Currently, surgeons involved with trauma, intestinal ischemia, short bowel syndrome, inflammatory bowel disease, and intestine transplantation have limited literature resources defining small bowel length in live humans [3-5]. Treatment guidelines and reviews quote the normal SBL as 275 cm to 850 cm with a mean ± sd of 350 ± 60 cm [1-6].
Intestinal length has been of interest since antiquity. Because of religious prohibitions and other societal limitations, little reliable data was generated until the first comprehensive study on non-preserved human cadavers by Sir Frederick Treves [7]. With current living subject and cadaver studies, it is often difficult to determine the measurement and accuracy of the results from these reports; some (SBL) length data in textbooks were derived from fresh or formalin-fixed cadaver studies, many from India [7-11].
Currently, it is not known whether the length of the small bowel as measured in formalin-fixed cadavers is equivalent to that in living humans. In our earlier study, the small bowel length was measured in live patients intraoperatively and compared to previously published SBL in living human subjects [1]. The hypothesis was that SBL in cadavers was shorter than in the living. The current study is unique because it used a standard method to measure SBL in both formalin-fixed cadavers and living subjects yielding a contemporaneous comparison. In addition, we studied whether there was any correlation between SBL and height, gender, and other body measurements, since there has been continuing debate in the literature about this issue [7-9,12].
Small bowel length was measured in 167 formalin-fixed human cadavers from three medical school anatomy labs to establish normal human cadaver ranges. Forty-nine subjects who had prior small intestinal surgery were excluded, leaving 118 cadavers with intact small bowel in the cohort. These measurements were compared to previously published in vivo human SBL data [11]. Additional external anatomic measurements were made to assess correlation with SBL. This study was approved by the Institutional Review Boards of each institution.
A search through PubMed, MedLine, and Google Scholar was undertaken to review published English literature on cadaveric and in vivo SBL for comparison with the study data.
Human cadaveric data was obtained in three medical school anatomy laboratories in formalin-fixed, un-frozen bodies using the same method, as taught by the principle investigator and observed in random cadavers to assure consistency. When the abdominal cavity was opened, the small bowel length was measured in situ along the anti-mesenteric border using a 25-cm umbilical tape. It was measured once from the Ligament of Treitz to the ileocecal valve. The bowel was serially measured with segmental straightening but without undue stretching. The principal investigator had performed all in vivo measurements. Cadaveric and in vivo measurements were completed consistently and without significant longitudinal traction so that the data collected could be reliably compared.
The following additional parameters and measurements were collected from the cadavers: gender, height, evidence of previous surgery, abdominal wall thickness at the umbilicus, the distance from the cricoid to the jugular notch, sternal angle, xiphoid, umbilicus, and pubic tubercle, and the torso circumference at the xiphoid-sternal angle, the costal margin, the umbilicus and the iliac crest. Cadaver heights and weights were recorded, when possible. No medical records were available for these subjects. Cadavers with prior abdominal incisions and any evidence of small intestinal surgery were excluded from statistical analysis.
New cadaveric data was compared to the earlier in vivo raw data in the report by Teitelbaum, et al. [11]. There were 287 de-identified subjects with in vivo SBL data available for comparison. This data had been collected during open laparotomies in living humans by the primary investigator using the same measurement technique, as previously described [11].
Statistical analysis was performed with the R v3.3.2 statistical software [13]. Analysis encompassed 118 cadavers, all numbered without relation to their cadaver identification number. Demographic characteristics including gender, age, and height were first compared in cadavers and living subjects. Fisher's exact test was used to determine gender; Welch's t-tests were used to compare groups on age and height. The total SBL was compared between the cadavers and the living subjects using nested generalized linear regression models. To examine whether age, height, gender, or a number of physical measurements might be related to small bowel length within the cadaver group, a series of analyses were conducted. First, correlations between age and total length, as well as height and total length were calculated and tested against zero. Similarly, correlations between the series of physical measurements and total length were calculated and tested against zero. A Welch's t-test was performed to determine if there were differences between genders. Lastly, nested linear models were constructed using age, height, and gender; the models were compared using Likelihood ratio tests.
Table 1 provides the summary age and height of the cadavers and living subjects in this study. The cadaver group included 57 (48%) women and 61 (52%) men. Age was available in 40% (47 of 118) of the cadavers. Ages ranged from 53 to 102 years, with a median age of 82 years. All but one of the cadavers had height information. Heights ranged from 145 cm to 199 cm, with a median of 174 cm. The in vivo group included 143 (50%) women and 144 (50%) men. Ages ranged from 14 to 95 years, with a median age of 56 years. Heights ranged from 138 cm to 196 cm, with a median of 168 cm. Comparisons of the two groups on basic demographics revealed no significant difference in gender (p = 0.83), but the cadavers were both older (p < 0.0001) and taller (p < 0.001).
Table 1: Age and height of the study cadavers and living subjects. View Table 1
For this reason, generalized linear models were used to examine the relationship between groupings (cadaver vs. living subjects) and total SBL, controlling for age and height. Nested models showed that cadavers have significantly shorter small bowel length than the living subjects (p < 0.0001), even when controlling for age and height (Table 2 and Figure 1).
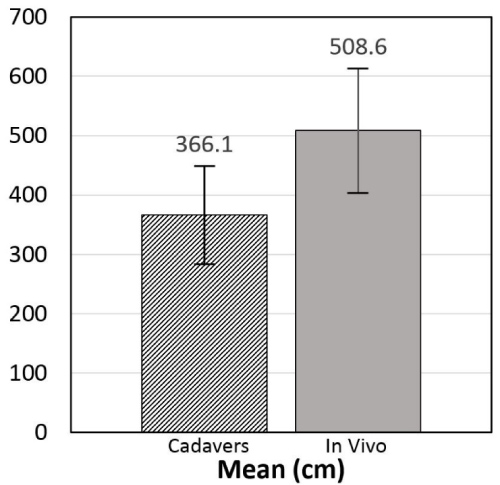 Figure 1: Mean SBL in formalin-fixed cadavers compared with in vivo subjects (n = 118 cadavers and 287 in vivo)-p < 0.0001. Normal small bowel length (SBL) means/ranges have been established. SBL was significantly longer in live subjects versus formalin-fixed cadavers. This finding is important for the transplant surgeon for small bowel transplantation, and other gastrointestinal surgical decisions.
View Figure 1
Figure 1: Mean SBL in formalin-fixed cadavers compared with in vivo subjects (n = 118 cadavers and 287 in vivo)-p < 0.0001. Normal small bowel length (SBL) means/ranges have been established. SBL was significantly longer in live subjects versus formalin-fixed cadavers. This finding is important for the transplant surgeon for small bowel transplantation, and other gastrointestinal surgical decisions.
View Figure 1
Table 2: Total small bowel length of cadavers and living subjects. View Table 2
Initial correlations and t-tests within the cadaver group indicated an inverse relationship between age and total SBL (Pearson's = -0.40; p = 0.006), and a direct relationship between height and total SBL (Pearson's = 0.42; p < 0.0001). Gender and total SBL were also related (t-test; p < 0.0001). Older people had shorter SBL; taller people had longer SBL; and men had longer SBL than women.
When multiple regression models were considered, the only variable that remained significantly correlated with SBL was height (p < 0.0001). Once height was controlled for, age (p = 0.51) and gender (p = 0.21) were no longer significantly related to total SBL. Age and height were negatively correlated (Pearson's correlation coefficient = -0.51; p = 0.001) and men were taller than women (t-test; p < 0.0001).
Table 2 shows SBL measured in 118 formalin-fixed human cadavers and 287 living subjects.
Many of the physical measurements were positively correlated with total SBL in cadavers (Table 3). Except for the abdominal wall thickness, the correlation between the SBL and circumference and bowel length at different levels was statistically significant (Table 4). These included measurements of length from the cricoid to the jugular notch, angle, xiphoid, umbilicus, pubic tubercle (p < 0.0001 top = 0.005). In addition, torso circumferences at the xiphoid-sternal angle, subcostal line, umbilicus, and iliac crest were also positively correlated with SBL (p < 0.0001 to p = 0.005).
Table 3: Summary statistics of all additional cadaver measurements (centimeters). View Table 3
Table 4: Pearson correlation coefficient between physical measurements and total small bowel length. View Table 4
The published studies were from Sweden, Italy, United States of America, United Kingdom, Thailand, Turkey, and France. Table 5 depicts the data available in the English literature for 7 reports of fresh cadaver small bowel measurement (1885-2012) for comparison with the present study [4,7-10,14,15]. The mean fresh cadaver SBL measurements ranged from 364 to 699 cm in contrast to measurement (mean 366.1 cm) done on the formalin-fixed cadavers in this report. There were 9 reports on in vivo SBL lengths (1974-2013) shown in Table 6 [9,11,16-23]. Table 7 depicts the SBL measuring process reported for the cadavers and intraoperative patients [4,7-11,14-23]. All SBL measurements were taken from the Ligament of Treitz to the ileocecal valve, except for Underhill [8] who included the pylorus in the measurement of the SBL. A variety of implements were used for measurement. Statements were made by most authors that the bowel was not intentionally stretched during the measurement process. Underhill and Hounnou, et al. [10] removed the bowel from the abdominal cavity measurement, introducing another confounding variable. Measurements were made along the antimesenteric border of the SB in the majority of studies. The number of cases ranged from 8 to 443 measured with tape, suture or ruler (SBL 428-824 cm). The longest SBL was reported in the study by Raines, et al. where a rigid 10 cm ruler was used (mean 998.5 cm) [23].
Table 5: Cadaver SBL measurements in the literature. View Table 5
Table 6: In Vivo intraoperative SBL measurements in the literature. View Table 6
Table 7: SBL Measurement Process in Cadavers and in vivo Subjects. View Table 7
This study indicated that when SBL was measured in the same consistent manner, the small bowel was shorter in formalin-fixed cadavers compared to living subjects and to previously published fresh cadavers. The present study also confirmed the findings by Gondolesi, et al. [4] in the in vivo SBL measurement; that data, however, was based on only 8 cadavers who were donors for intestinal transplantation.
Although there were correlations between cadaveric SBL and many other measurements such as torso circumference and various longitudinal subject lengths, overall height was the best predictor of SBL. Underhill [8] and Gondolesi, et al. [4] also found a positive correlation with height.
Similarly, this correlation with height was found in our in vivo study subjects [11]. Literature on correlations between SBL and other body measurements is mixed. Underhill [8] found that intestinal length was correlated with height but independent of age, as we did. However, Hounnou, et al. [10] found body weight was significantly correlated with SBL. Tacchino, et al. [23] analyzed the relationship of SBL to obesity and did not find it significant. Earlier reports found no correlation with age, height, or weight [7-9,14].
In an interesting study, Gondolesi, et al. [4] evaluated the ratio of small bowel length to body surface area (BSA) in children. There were 2 groups: Group 1 (number = 5) with a height of < 70 cm with an age of 0.58 ± 0.21 years; and Group 2 (number = 5) with a height of > 70 cm --- < 150 cm and an age of 5.6 ± 2.51 years. They found that SBL did not increase with growth, and so the SBL/height ratio decreased with growth, concluding that SBL was fairly constant after childhood. In agreement with this study, age was not significant when height was included in the model in our study.
A strength of this study is that a standardized and reproducible method of small bowel measurement was utilized in both in vivo and cadaveric subjects. Additionally, the number of cadavers examined was larger than in other published studies; the number of in vivo subjects was also the highest yet reported.
The results of this investigation indicate that the SBL is shorter in formalin-fixed cadavers compared to living subjects. This is supported by Table 7, where the average of the fresh cadaveric SBLs (592.8 cm) is longer in comparison to the formalin-fixed cadaver SBL (366 cm). To date, this study remains the first to compare detailed physical measurements to SBL (Table 3 and Table 4). These anthropometric indices in these two tables are directly associated with height, therefore, it makes sense they are significant correlators with SBL. Future studies may focus on whether individual anthropometric indices independently correlate with SBL in both cadaveric and in vivo subjects.
There are many artifacts that may affect SBL other than the reported elements, temperature, and opioids, such as the formalin-fixation process, genetics, chronic diseases, and nutritional status before death [9,24]. Crohn's disease was considered an independent risk factor for shortened small bowel in two studies [18,19]. To our knowledge, none of the subjects in this study had Crohn's disease. Earlier reports described a loss of muscular tonicity after death resulting in increased length [8,12] while another study [24] described an intestinal retraction phenomenon that resulted after surgical intestinal resection. The retraction phenomenon did not occur in cadavers, but rather in colorectal resection specimens from live patients [24]. It is possible that the small bowel in fresh cadavers is significantly longer with relaxation of the smooth muscle and that this is reversed by the formalin-fixation process. Goldstein, et al. [24] noted that in surgical colorectal specimens, there was a 40% reduction of length in formalin-fixed tissue compared to the prior in vivo lengths. This may explain why the mean SBL in the formalin-fixed cadavers in the current study was only 63% as long as the SBL in in vivo subjects (mean 366.1 vs. 508.6 cm). In contrast, fresh cadaver SBLs in the literature were longer compared to the in vivo and the formalin-fixed SBL measurements in this study. Overall, our in vivo SBL lengths were consistent with the SBL lengths reported in the literature (Table 6).
Limitations of this study primarily include the wide variation in age. In addition, although we recognize a larger study population would improve the power, our study remains the largest analysis of a cadaveric population to date. In our data, 60% of the cadavers did not have an age recorded, and so the mean and median ages listed may not be accurate. Perhaps with a larger cohort, age may be correlated with SBL. Many intestinal and abdominal disorders may have an effect on small bowel length; these could not be identified from the cadavers. The circumference measurements may be associated with weight, but it was not possible to get accurate cadaver weights and body mass index (BMI).
It is essential for the clinician to have a good understanding of normal small bowel length and ranges since this has implications in many clinical situations such as trauma, small bowel transplantation, intestinal bypass, Roux-en-y reconstruction, small bowel Crohn's disease, intestinal ischemia, and short bowel syndrome. With the current trend of utilizing living donor small bowel transplant (LR-SBTx) of the terminal ileum, it is important to have accurately estimated donor SBL so that the donors can retain the recommended 60% of their SBL for survival and freedom from post-donation intestinal complications [25]. To reduce error in SBL length measurement, a recommendation from an in vivo healthy liver donor study was to perform several measurements on stretched compared to non-stretched bowel [26]. Trauma and Gastrointestinal surgeons should be vigilant in preserving small bowel, especially in patients with shorter than average height. Fresh or formalin-fixed cadaveric SBL data do not provide good estimates of SBL in living human subjects.