Chronic Rotator Cuff Tears (RCT) are a common and disabling condition. Local tissue changes may be assessed by Infrared Thermography (IRT). It was hypothesized that IRT might provide useful information for diagnosis of chronic RCT, yielding lower local skin temperatures.
Included patients consisted of adults with chronic primary RCT (> 3 months). Demographics and occupation were recorded. An IRT protocol was used, at rest and after exercise, for both affected and contralateral shoulder. Frontal, dorsal and lateral views were used, and Regions of Interest (ROI's) were defined in the topography of the main rotator cuff tendons. Three independent observers assessed temperature, and concordance analysis was performed. Significant temperature variation was defined as 0.5 ℃.
52 patients - 16 males and 36 females - were evaluated, mean age 56 ± 1.3 years old. Inter-observers' concordance was greater than 95%. A slight decrease in temperature was verified after the exercise protocol in affected and contra-lateral shoulders, but this was less than 0.5 ℃. Comparing the skin temperature of affected shoulders and contralateral temperatures, no significant differences were revealed, both at rest or after exercise.
The obtained results demonstrated IRT as highly reproducible. A small decrease in skin temperature after exercise has been related to peripheral vasoconstriction, and this was confirmed in both affected and non-affected shoulders. Nevertheless, it was expected on affected shoulders a lower baseline and after exercise skin temperatures, which was not confirmed, as no significant difference was found between groups. As such, the role of IRT as complimentary mean of diagnosis is yet to be established in RCT.
Thermography, Rotator Cuff Tears, Thermal Imaging, Cuff Tear Diagnosis, Rotator Cuff Imaging
RCT: Rotator Cuff Tear; IRT: Infrared Thermography; BMI: Body Mass Index; NETD: Non-Equivalent Temperature Difference; ROI: Regions of Interest; VAS: Visual Analogue Scale; DASH: Disabilities of the Arm, Shoulder and Hand; ICC: Intraclass Correlation Coefficient
Rotator Cuff Tears (RCT) are a disabling condition affecting a considerable group of the adult population [1]. They comprise tears of the Supraspinatus, Infraspinatus, Subscapularis and, less often, the Teres Minor. RCT are commonly caused by a degenerative condition and may develop with or without symptoms throughout long periods until chronicity. Despite the considerable amount of literature focusing on this topic, the definition of a chronic RCT is still controversial [2], and issues regarding inflammation, degeneration, and symptomatic correlation are still difficult to assess. Progressive degenerative muscle changes such as atrophy and fatty infiltration are a common recognized consequence of chronic rotator cuff tears [3,4], together with a decrease in muscle activity. Some authors found that this may have an important effect in the capillary network [5,6], which may also be influenced by changes in inflammatory patterns [7-9].
Several complementary means od diagnosis are available for assessment of chronic RCT, although often not correlating with the severity of symptoms [10]. Infrared Thermography (IRT) is a portrait of skin temperature distribution, which is related to peripheral blood flow in a given area [11]. Its use has been widely studied in several fields of medical sciences, including orthopedic conditions [12]. Therefore, it can detect local variations in temperature, as it may occur in certain conditions affecting the musculoskeletal system [13], including shoulder injuries such as chronic RCT, due to changes in the local capillary system. The rationale for this study was that IRT might add as a simple, innocuous and inexpensive means of diagnosis, allowing assessment of these temperature variations, although there is still scarce literature regarding its use in RCT.
The aim of this research was to evaluate the IRT reproducibility in shoulder temperature evaluation, and assess its correlation with the presence of chronic RCT. The hypothesis is that IRT might be able to detect thermal changes in shoulders affected by chronic RCT, and that these changes would be reflected through lower local skin temperature.
A cross-sectional study was designed to assess IRT in the diagnosis of RCT. Patients were included according to the following criteria: 1) Over 18 years-old; 2) Symptomatic full-thickness RCT, confirmed with Magnetic Resonance Imaging (MRI); 3) More than 3 months from the confirmatory MRI; 4) No previous history of shoulder surgery, systemic inflammatory or neoplastic diseases. Exclusion criteria were: 1) Bilateral involvement; 2) Active infection; 3); 4) Irreparable RCT (Goutalier > II, diameter > 5 cm); 5) Shoulder pseudoparalysis; 6) Shoulder stiffness (restricted passive range of motion; 7) Rotator cuff repair performed before evaluation; 8) Refusal to enroll in all evaluation procedures. The Ethical Committee of the senior author's institution analyzed and approved the research, and all participants signed an informed consent form.
Demographics were assessed for each patient - gender, age, occupation (white or blue collar) and Body Mass Index (BMI). Data regarding subjective pain evaluation was evaluated through the Visual Analogue Scale (VAS). Global shoulder function was estimated through the Constant and Murley score and the Disabilities of Arm and Shoulder score (DASH).
Patients were requested not to smoke, drink alcohol, intake heavy meal or hot drinks, use transdermal medication in the shoulder region for, at least, four hours before evaluation. Thermography records were performed in a controlled environment with constant temperature (22 ℃), after a 15-minute calibration period, without any covering of the shoulder, neck and back regions. A FLIR A325 camera (FLIR® - Wilsonville, Oregon, USA) was used. This device has a focal plane array thermal sensor size of 320 × 240, operating in a long wave infrared and detecting a range of temperature that goes from -20 ℃ to + 120 ℃. It has a Non-Equivalent Temperature Difference (NETD) of 50 mK at 30 ℃ and a measurement uncertainty ± 2% of the overall reading temperature range. The infrared thermal camera was calibrated using a Isotech (Isotech® - Southport UK) Hyperion R Model 982 blackbody immediately before and at the end of each examination day for quality assurance purpose.
The camera was maintained approximately 1.0 meter from the shoulder joint mounted in a tripod to avoid angle changes. Readings were performed in both shoulders from frontal, dorsal and lateral views at baseline and after an exercise protocol. This comprised 15 active abduction repetitions in the scapula plane, from 0 to 90°, in neutral rotation. Exercises were performed with both shoulders simultaneously [14]. IRT was assessed following an established protocol [15].
For the assessment of the RCT, we adopted an anatomical classification according to Middleton [16], defining the Regions of Interest (ROIs), circle over the skin area, which overlaps the tear (ROI1) in anterior, posterior and lateral views, and two rectangles in the skin areas that superimpose the main superior (ROI2) and inferior (ROI3) tendons, which connect the tear, at the anterior and dorsal views.
In the frontal and dorsal views, temperature was measured in two Regions of Interest (ROI), and in the lateral view, assessment was made in one ROI, as shown in Figure 1. The circle ROI identifies the shoulder region. Each rectangle aims to reproduce the topographic location of the main rotator cuff tendons. Three independent observers defined temperature value in the circle region, as it is considered the most relevant.
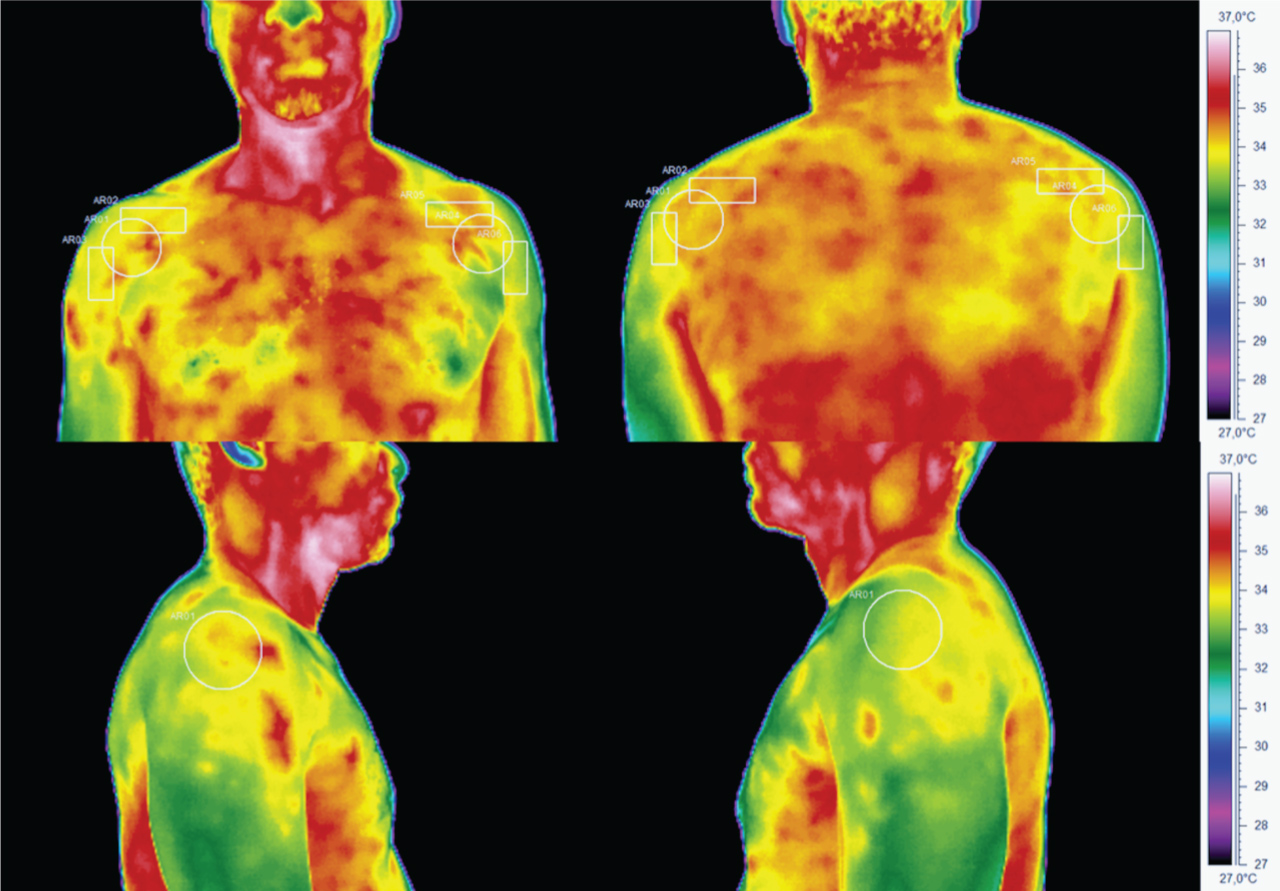 Figure 1: Incidences and Regions of Interest in thermographic analysis. View Figure 1
Figure 1: Incidences and Regions of Interest in thermographic analysis. View Figure 1
Statistical analysis was performed using IBM SPSS Statistics, version 22 (IBM® Corp., Armonk, N.Y., USA). Descriptive statistics were performed. Continuous variables were assessed for normality (Shapiro-Wilk test) and, if normally distributed, parametric tests were used. Inter-observer concordance was tested with the Intraclass Correlation Coefficient (ICC) (Two-way mixed agreement). Temperature differences in the involved and uninvolved shoulder were calculated both in rest and after exercise protocol and independent samples t-test were applied. Temperature variation after exercise in the same shoulder was also verified using paired samples t-test. Significant temperature variation was considered when absolute value is above 0.5 ℃. This cut-off point temperature is based in the related temperature [17-19], which suggests this value as a valid threshold between health and pathological states. One sample t-tests were performed to assess if absolute variation was significantly different from this threshold. Statistical significance was considered for p values under 0.05.
This study evaluated and approved by the S. João University Hospital Ethical Committee.
Overall, 52 patients - 16 males and 36 females - were enrolled in this study after fulfilling selection criteria. Demographics are shown in Table 1. Most patients (78%) were involved in Blue Collar occupations. The right shoulder was most commonly affected (65%). Mean patients' age was 56.6 years-old ± 1.3 and mean BMI was 28.5 kg/m2 ± 0.7.
Table 1: Descriptive statistics for categorical variables. View Table 1
The mean VAS was 6.4 ± 0.3, the mean DASH score was 42.1 ± 19.6 and mean Constant score was 31.6 ± 17.1.
Concordance analysis revealed high concordance coefficients between observers in all measurements, performed in different incidences and ROIs (Graphic 1). These measurements were considered as accurate and thus validated the use of the mean temperature assessed by each observer in the analyses further performed.
 Graphic 1: Intraclass concordance coefficient between observers. View Graphic 1
Graphic 1: Intraclass concordance coefficient between observers. View Graphic 1
Absolute skin temperature values are presented in Table 2. Skin temperature assessment and variation before and after a standardized exercise program are presented in Figures 2A, Figure 2B and Figure 2C, according to the different incidences used in IRT analysis.
Table 2: Absolute skin temperature values (℃) recorded by Infrared Thermography (mean and standard deviation). ROI - Region of Interest. View Table 2
 Figure 2A: Skin temperature before and after a standardized exercise protocol, in the different regions of interest (ROI). Black line - affected shoulder. Red line - unaffected shoulder.
Figure 2A: Skin temperature before and after a standardized exercise protocol, in the different regions of interest (ROI). Black line - affected shoulder. Red line - unaffected shoulder.
Figure 2A: Frontal Incidence.
View Figure 2A
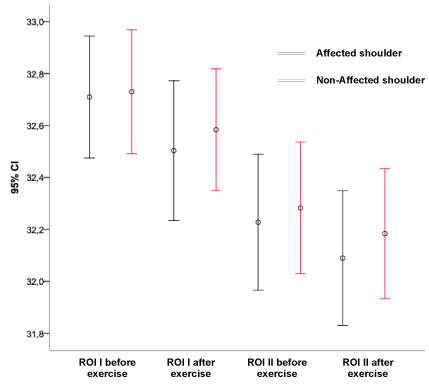 Figure 2B: Dorsal incidence. View Figure 2B
Figure 2B: Dorsal incidence. View Figure 2B
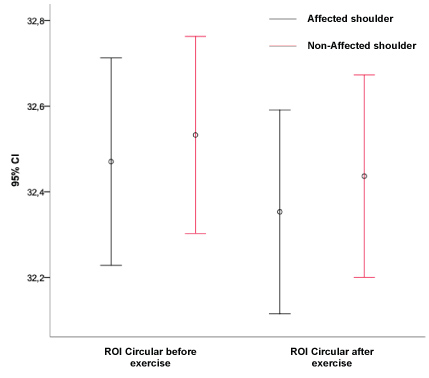 Figure 2C: Lateral incidence. View Figure 2C
Figure 2C: Lateral incidence. View Figure 2C
Graphics' analysis demonstrates that there is no significant difference in temperature between the normal and affected shoulder, both in resting and after exercise.
Skin temperature variation was calculated for all incidences, as the difference between the one recorded before and after the exercise protocol. One sample t-test for temperature variation has shown a tendency for decreasing temperature after the exercise protocol, and this was considered statistically significant, in all the considered incidences in both affected and unaffected shoulders (Table 3). Nevertheless, the difference was below 0.5 ℃, in affected as well as unaffected shoulders (Figure 3).
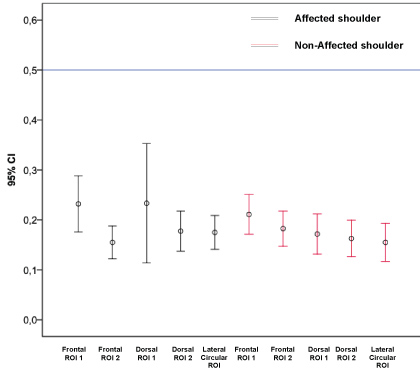 Figure 3: Absolute temperature variation after the exercise protocol in affected and unaffected shoulders - position to the significant variation of 0.5 ℃. View Figure 3
Figure 3: Absolute temperature variation after the exercise protocol in affected and unaffected shoulders - position to the significant variation of 0.5 ℃. View Figure 3
Table 3: Temperature variation (℃) in each ROI before and after the exercise protocol. Values were significantly different from 0. ROI - Region of Interest. View Table 3
Rotator cuff tears are a common and disabling condition, but it seems that there is only a poor correlation between the duration of symptoms and features like the physical examination tests for strength, the patient reported level of pain, or even the severity of the rotator cuff tear, and patients with large tears may become asymptomatic, while others with smaller tears may show significant impairment [2]. Thermography has been studied in the diagnosis and treatment of patients with other chronic musculoskeletal conditions [20,21], including shoulder pathology [22], but its definite role has not yet been established.
Our results have shown that shoulder temperature assessment is highly reliable between observers, as high concordance coefficients were obtained for every ROI. Other studies [19,23,24] have evaluated the reproducibility of this method, and also supported a high degree of internal validity in temperature measurement using this method. This confirms that several observers can perform IRT analysis without affecting the accuracy of measurements, thereby facilitating its use.
In healthy individuals, skin temperature has been described as equal in both sides of the body [17,23], and an asymmetry has been associated with pathological conditions [23,25]. Therefore, this study aimed to evaluate if chronic rotator cuff tears had an effect detected by IRT in skin temperature, reflecting the reduced activity and degenerative condition of the tendons in this area. Both affected and unaffected shoulders demonstrated lower skin temperature after an exercise protocol. Several studies assessed the effect of different types of exercise in skin temperature and found that in low intensity activity, skin temperature decreased during exercise, as well as during the initial phase of high intensity anaerobic programs [26,27]. They correlated this to an effect of peripheral vasoconstriction for enhanced muscle blood supply. This effect may explain our findings of temperature decrease after exercise, even if subtle and below the threshold considered for a pathologic asymmetry (0.5 ℃).
When comparing the two groups – RCT and non-RCT shoulders - for their skin temperature at baseline and after exercise, it was not possible to identify a significant asymmetry. This differs from the conclusions of the literature evaluating thermography in other shoulder pathologies such as "frozen shoulder" or "impingement syndrome". Jeracitano, et al. [25] studied the thermal response after a cold challenge and found a significant decrease during the rewarming phase in "frozen shoulders", as these failed to return to basal values. They suggested an autonomic nervous system dysfunction, associated with fibrotic changes of the shoulder joint. Chronic rotator cuff tears are also associated with muscle atrophy, fatty infiltration and fibrosis [28], and our study may point out for a lack of a strong dysautonomic effect of the shoulder condition in local tissues. On the other hand, Park, et al. [22] compared patients with shoulder impingement syndrome with a group of healthy controls and could not identify a correlation between inflammation or pain with thermography, although there was an association of local hypothermia and decreased range of motion. This may point out that vasomotor changes around the shoulder are less relevant in this kind of conditions or may simply not be reflected in skin temperature. Another study assessed skin thermal changes in rotator cuff tendinitis [29] and could not identify a specific pattern, suggesting that the current methods may be unable to detect the low-grade inflammatory process. Literature concerning this topic in rotator cuff tears is scarce and no studies were found for comparison, but a lack of a detectable change in skin temperature appears to be more likely when considering low-grade inflammatory or degenerative conditions of the shoulder. In addition, the shoulder is a multi-layered region with a thick muscular covering, such as the deltoid and the pectoralis major, which may impair the detection of thermal changes that may occur in the underlying rotator cuff. Although other studies attempted to use IRT in deep shoulder conditions (eg rotator cuff tendinitis and impingement syndrome) [22,25,29], these anatomical constraints may be detrimental in IRT evaluation.
We acknowledge the limitations of this study. A small and heterogeneous sample was evaluated, and elapsed time from the onset of the symptoms is missing, as this can influence the inflammation associated with the cuff tear. Recordings were not performed in a strict laboratory environment, but standard procedures from the Guidelines for Neuromuscular Thermography [15,30,31] were adopted and a high reliability in measurements was found. There are several confounding factors for these measurements, especially when trying to understand the influence of non-subcutaneous structures, as soft tissue envelope may overpower the results. Further studies may focus on potential differences between acute and chronic tears, and other characteristics such as number of involved tendons may affect local temperature changes in this pathology.
This study suggests that at present, despite being an important source of reliable measurements, IRT could not identify changes associated with chronic RCT, and thus its complimentary diagnostic role is still to be established in this condition. For further investigation, a larger sample with control of the onset of symptoms and using a thermal stimulus instead of a physical provocation is advised to overcome this conclusion.
The co-author, Ricardo Vardasca, acknowledges the partial funding of Project NORTE-01-0145-FEDER-000022 - SciTech - Science and Technology for Competitive and Sustainable Industries, financed by Programa Operacional Regional do Norte (NORTE2020), through Fundo Europeu de Desenvolvimento Regional (FEDER) and the FCT - Foundation for Science and Technology under the project (PEst-OE/EME/LA0022/2013).