Chronic prostatitis (CP) is an internationally important health problem of the man, particularly in developed countries. The aim of this exploratory study was to evaluate whether significant changes in the levels of Zn and some other trace elements of prostatic fluid exist in the inflamed prostate.
Prostatic fluid levels of Br, Fe, Rb, Sr, and Zn were prospectively evaluated in 33 patients with CP and 42 healthy male inhabitants. Measurements were performed using 109Cd radionuclide-induced energy dispersive X-ray fluorescent microanalysis. Prostatic fluid samples were divided into two portions. One was used for cytological and bacteriological investigations while the other was intended for trace element analysis.
Mean values ± standard error of means (M ± SΕΜ) for concentration (mg/L) of trace element in the expressed prostatic fluid (EPF) of normal prostate were: Br 2.86 ± 0.59, Fe 8.30 ± 1.42, Rb 1.16 ± 0.10, Sr 1.27 ± 0.17, and Zn 598 ± 34. It was observed that in the EPF of inflamed prostate content of Rb significantly increased whereas content of Zn decreased in a comparison with those in the EPF of normal prostate.
There are significant changes in trace element contents and their relationships in the fluid of CP prostate. The alterations in levels of Zn and Rb in the EPF of inflamed prostate might demonstrate an involvement of these trace elements in etiology and pathogenesis of CP. It was supposed that the changes of Zn and Rb levels in the EPF samples can be used as CP markers.
Chronic prostatitis, Prostatic fluid, Trace elements, Energy-dispersive X-ray fluorescent analysis
Chronic prostatitis (CP) is functional, somatoform disorder with a high worldwide prevalence estimated in systematic reviews or population studies at 10-32% [1-5]. However, CP is a more common condition, with 35-50% of men reported to be affected by symptoms suggesting prostatitis during their lifetime [6,7].
CP is characterized by a multifactorial pathogenesis, and these conditions are defined on the basis of clinical presentation rather than clear diagnostic markers or findings [8]. The absence of robust and clear diagnostic markers may the overlap of CP symptoms with other conditions, such as benign prostatic hyperplasia and prostate cancer.
Oxidative stress has a significant involvement in the pathogenesis of CP [9]. Oxidative stress is a result of the imbalance between reactive oxygen species and antioxidants, including some trace elements, in the body that can cause tissues and organs damage. Trace elements, besides their antioxidant properties, have many other essential physiological functions such as maintenance and regulation of cell function, gene regulation, activation or inhibition of enzymatic reactions, and regulation of membrane function. Essential or toxic (mutagenic, carcinogenic) properties of trace elements depend on tissue-specific need or tolerance, respectively [10,11].
In our previous studies a significant involvement of Zn, Ca, Mg, and, perhaps, Rb and some other trace element in the function of prostate was observed [12-22]. One of the main functions of prostate gland is a production of prostatic fluid [23] with extremely high concentration of Zn and elevated level of Ca, Mg, Rb, and some other chemical elements in a comparison with those in serum and other fluids of human body. Prostatic fluid is main liquid portion of semen (about 30-35% of the semen ejaculate) and the composition of the prostatic fluid is vital for the well-being of the sperm cells after ejaculation.
The first finding of remarkable high level of Zn concentration in human expressed prostatic fluid (EPF) was reported in the beginning of 1960s [24]. Analyzing EPF expressed from prostate of 8 apparently healthy men aged 25-55 years it was found that Zn concentration varied in range from 300 to 730 mg/L. After this finding several investigators have suggested that the measurement of Zn level in EPF may be useful as a marker of prostate secretory function [25,26]. It promoted a more detailed study of Zn concentration in EPF of healthy subjects and in those with different prostate diseases, including CP [26,27]. A detailed review of these studies, reflecting the contradictions within accumulated data, was given in our earlier publication [27]. Additionally, some recent evidences have showed a significant association between CP and male infertility including a detrimental effect on sperm parameters, such as low level of Zn concentration in semen and others [28].
Thus, data on changes of trace element contents in EPF of patients with CP are very important, because it can clarify our knowledge of CP and male infertility pathogenesis and may be useful as CP diagnostic markers. In present study it was supposed by us that apart from Zn the levels of some other trace elements in EPF have to reflect a disturbance of prostate function. Thus, this work had four aims. The first one was to present the design of the method and apparatus for microanalysis of Br, Fe, Rb, Sr, and Zn in the EPF samples using energy dispersive X-ray fluorescence (EDXRF) with radionuclide source 109Cd. The second aim was to assess the Br, Fe, Rb, Sr, and Zn concentration in the EPF samples obtained from patients with CP. The third aim was to evaluate the quality of obtained results and to compare obtained results with published data. The last aim was to compare the concentration of Br, Fe, Rb, Sr, and Zn and intercorrelations of these trace elements in EPF samples of normal and inflamed prostate gland.
Specimens of EPF were obtained from 42 men with apparently normal prostates (mean age ± Standard Deviation - 54 ± 13 years, range 31-75 years) and from 33 patients with CP (mean age 50 ± 9 years, range 37-65 years) by qualified urologists in the Urological Department of the Medical Radiological Research Centre using standard rectal massage procedure. In all cases the diagnosis has been confirmed by clinical examination and by cytological and bacteriological investigations of EPF samples. Subjects were asked to abstain from sexual intercourse for 3 days preceding the procedure. Specimens of EPF were obtained in sterile containers which were appropriately labeled. Twice twenty μL (microliters) of fluid were taken by micropipette from every specimen for trace element analysis, while the rest of the fluid was used for cytological and bacteriological investigations. The chosen 20 μL of the EPF was dropped on 11.3 mm diameter disk made of thin, ash-free filter papers fixed on the Scotch tape pieces and dried in an exsiccator at room temperature. Then the dried sample was covered with 4 μm Dacron film and centrally pulled onto a Plexiglas cylindrical frame (Figure 1).
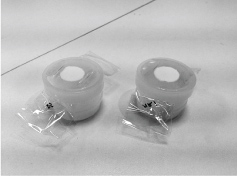 Figure 1: The dried samples of prostate fluid on filter paper disks fixed on the Scotch tape pieces centrally pulled onto a Plexiglas cylindrical frame. View Figure 1
Figure 1: The dried samples of prostate fluid on filter paper disks fixed on the Scotch tape pieces centrally pulled onto a Plexiglas cylindrical frame. View Figure 1
To determine concentration of the elements by comparison with a known standard, aliquots of solutions of commercial, chemically pure compounds were used for a device calibration [29]. The standard samples for calibration were prepared in the same way as the samples of prostate fluid. Because there were no available liquid Certified Reference Material (CRM) ten sub-samples of the powdery CRM IAEA H-4 (animal muscle) were analyzed to estimate the precision and accuracy of results. Every CRM sub-sample weighing about 3 mg was applied to the piece of Scotch tape serving as an adhesive fixing backing. An acrylic stencil made in the form of a thin-walled cylinder with 11.3 mm inner diameter was used to apply the sub-sample to the Scotch tape. The polished-end acrylic pestle which is a constituent of the stencil set was used for uniform distribution of the sub-sample within the Scorch surface restricted by stencil inner diameter. When the sub-sample was slightly pressed to the Scotch adhesive sample, the stencil was removed. Then the sub-sample was covered with 4 μm Dacron film. Before the sample was applied, pieces of Scotch tape and Dacron film were weighed using analytical balance. Those were again weighed together with the sample inside to determine the sub-sample mass precisely.
The facility for radionuclide-induced energy dispersive X-ray fluorescence included an annular 109Cd source with an activity of 2.56 GBq, Si(Li) detector with electric cooler and portable multi-channel analyzer combined with a PC. Its resolution was 270 eV at the 6.4 keV line. The facility functioned as follows. Photons with a 22.1 keV 109Cd energy are sent to the surface of a specimen analyzed inducing the fluorescence Kα X-rays of trace elements. The fluorescence irradiation got to the detector through a 10 mm diameter collimator to be recorded.
The duration of the Zn concentration measurement was 10 min. The duration of the Zn concentration measurement together with Br, Fe, Rb, and Sr was 60 min. The intensity of Kα-line of Br, Fe, Rb, Sr, and Zn for EPF samples and standards was estimated on calculation basis of the total area of the corresponding photopeak in the spectra.
All EPF samples for EDXRF were prepared in duplicate and mean values of trace element contents were used in final calculation. Using the Microsoft Office Excel programs, the summary of statistics, arithmetic mean, standard deviation, standard error of mean, minimum and maximum values, median, percentiles with 0.025 and 0.975 levels was calculated for trace element concentrations in EPF of normal and PC prostate. The difference in the results between two groups of samples (normal prostate and CP) was evaluated by the parametric Student's t-test and non-parametric Wilcoxon-Mann-Whitney U-test. For the estimation of the Pearson correlation coefficient between different pairs of the trace element concentration in prostate fluid of health men and patients with CP the Microsoft Office Excel program was also used.
Table 1 depicts our data for Br, Fe, Rb, Sr, and Zn mass fractions in ten sub-samples of CRM IAEA H-4 (animal muscle) certified reference material and the certified values of this material. Of 4 (Br, Fe, Rb, and Zn) trace elements with certified values for the CRM IAEA H-4 (animal muscle) we determined contents of all certified elements (Table 1). Mean values (M ± SD) for Br, Fe, Rb, and Zn were in the range of 95% confidence interval. Good agreement of the trace element contents analyzed by 109Cd radionuclide-induced EDXRF with the certified data of CRM IAEA H-4 (Table 1) indicate an acceptable accuracy of the results obtained in the study of the prostatic fluid presented in Table 2, Table 3, Table 4 and Table 5.
Table 1: EDXRF data of Br, Fe, Rb, Sr, and Zn contents in the IAEA H-4 (animal muscle) reference material compared to certified values (mg/kg, dry mass basis). View Table 1
Table 2 presents certain statistical parameters (arithmetic mean, standard deviation, standard error of mean, minimal and maximal values, median, percentiles with 0.025 and 0.975 levels) of the Br, Fe, Rb, Sr, and Zn concentrations in EPF of normal and CP prostate.
Table 2: Some basic statistical parameters of Fe, Zn, Br, Rb, and Sr concentration (mg/L) in prostate fluid of health men and patients with prostatitis. View Table 2
The comparison of our results with published data for Br, Fe, Rb, Sr, and Zn concentrations in EPF of normal and CP prostate [26,27,30-32] is shown in Table 3.
Table 3: Median, minimum and maximum value of means of Fe, Zn, Br, Rb, and Sr concentration (mg/L) in prostate fluid of health men and patients with prostatitis according to data from the literature. View Table 3
The ratios of means and the differences between mean values of Br, Fe, Rb, Sr, and Zn concentrations in EPF of normal and CP prostate are presented in Table 4.
Table 4: Comparison of mean values (M ± SEM) of Br, Fe, Rb, Sr, and Zn concentration (mg/L) in prostate fluid of health men and patients with prostatitis. View Table 4
Table 5 contains results of inter-element correlation calculations (values of r - coefficient of correlation) including all trace elements identified in this work.
Table 5: Intercorrelations of pairs of the trace element concentration in prostate fluid of health men and patients with prostatitis (r - coefficient of correlation). View Table 5
The mean values and all selected statistical parameters were calculated for 5 trace elements (Br, Fe, Rb, Sr, and Zn) of trace element concentrations (Table 2). The concentrations of Br, Fe, Rb, and Zn were measured in all, or a major portion of EPF samples of normal and CP prostate. The Sr concentration was measured in major portion of EPF samples of normal prostate and in a few samples of CP prostate.
The mean values and all selected statistical parameters were calculated for 5 trace elements (Br, Fe, Rb, Sr, and Zn) of trace element concentrations (Table 2). The concentrations of Br, Fe, Rb, and Zn were measured in all, or a major portion of EPF samples of normal and CP prostate. The Sr concentration was measured in major portion of EPF samples of normal prostate and in a few samples of CP prostate.
In the EPF samples of CP prostate our results were comparable with published data for Zn concentrations (Table 3). No published data referring to Br, Fe, Rb, and Sr concentrations in EPF samples obtained from patients with CP were found.
A number of values for Zn concentrations in normal EPF were not expressed on a wet mass basis in the cited literature. Therefore, we calculated these values using the published data for water -93.2% [33].
From Table 4, it is observed that in EPF of CP prostate the concentrations of Rb is 2 times higher whereas the concentrations of Zn is 32% lower than levels of these trace element in EPS of normal prostate.
Inter-element correlations between trace elements are significantly altered in EPF of CP prostate as compared to their relationships in EPF of normal prostate (Table 5). In EPF of CP prostates some significant correlations between trace elements found in the EPF of control group are no longer evident but other correlations arise. For example, in the EPF of healthy males there is inverse correlation between Zn and Br (Table 5). Thus, if we accept the relationships of trace element concentrations in EPF of males in the control group as a norm, we have to conclude that with CP the relationships between trace elements in EPF significantly changed. No published data referring to correlations between trace elements concentrations in EPF of normal and CP prostate were found.
The range of means of Zn concentration reported in the literature for normal EPF (from 47.1 to 5185 mg/L) and for EPF of untreated CP prostate (from 88.9 to 564 mg/L) varies widely (Table 3). This can be explained by a dependence of Zn content on many factors, including age, ethnicity, mass of the gland, presence of benign prostatic hyperplasia, and others. Not all these factors were strictly controlled in cited studies. Another and, in our opinion, leading cause of interobserver variability was insufficient quality control of results in these studies. In many reported papers EPF samples were dried at high temperature or acid digestion. There is evidence that by use of these methods some quantities of trace elements, including Zn, are lost as a result of this treatment [34-36].
Characteristically, elevated or deficient levels of trace elements and electrolytes observed in EPF are discussed in terms of their potential role in etiology of diseases. In our opinion, abnormal levels of many trace elements in EPF of CP prostate could be the consequence of inflammation. Compared to other fluids of human body, the prostate secretion has higher levels of Zn and some other trace elements. These data suggest that these elements could be involved in functional features of prostate. Inflammation is accompanied by a suppression of specific functional activity of prostatic cells, which leads to a small reduction in the Zn content in EPF. Why Rb content increases in the CP prostate and how it acts on the gland are still to be fully understood.
Our findings show that the concentration of Rb is significantly higher whereas the concentration of Zn is somewhat lower in EPF of CP prostate as compared to their levels in EPF of normal prostate (Table 4). Thus, it is plausible to assume that levels of these trace elements in EPF can be used as CP markers. However, this subject needs in additional studies.
This study has several limitations. Firstly, analytical techniques employed in this study measure only five trace element (Br, Fe, Rb, Sr and Zn) concentrations in EPF. Future studies should be directed toward using other analytical methods which will extend the list of chemical elements investigated in EPF of normal and CP prostate. Secondly, the sample size of CP group was relatively small. It was not allow us to carry out the investigations of trace element contents in CP group using differentials like age, stage of disease, dietary habits of healthy persons and patients with CP, and others. Despite these limitations, this study provides evidence on inflammation -specific Rb and Zn level alteration in EPF and shows the necessity the need to continue chemical element research of EPF in norm and prostatic diseases.
In this work, trace elemental measurements were carried out in the EPF samples of normal and CP prostate using non-destructive instrumental EDXRF micro method developed by us. It was shown that this method is an adequate analytical tool for the non-destructive determination of Br, Fe, Rb, Sr, and Zn concentration in the EPF samples of human prostate. It was observed that in the EPF of CP prostate content of Rb significantly increased whereas content of Zn decreased in a comparison with those in the EPF of normal prostate. In our opinion, the alterations in levels of Zn and Rb in the EPF of inflamed prostate might demonstrate an involvement of these trace elements in etiology and pathogenesis of CP. It was supposed that the changes of Zn and Rb levels in the EPF samples can be used as CP markers.
We are grateful to Dr Tatyana Sviridova, Medical Radiological Research Center, Obninsk for supplying EPF samples.
All studies were approved by the Ethical Committees of the Medical Radiological Research Centre, Obninsk. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.