Surgical coverage of mandibular lingual recession is not a routinely implemented treatment procedure because of its lack of esthetic significance, which is one of the most common indications for recession coverage. A gold standard for recession coverage, the sub epithelial connective graft is used in conjunction with a novel modification of the tunneling technique to treat the lingual recession on mandibular anterior teeth.
A 33-year-old male patient with a previous history of smokeless tobacco, presented with pain, irritation and recession in the mandibular lingual area. #23 showed 4mm Millers Class 2 lingual recession. Surgical procedure consisted of making a sub periosteal tunnel from #23-26 and placing a sub epithelial connective graft harvested from the palate within the tunnel and securing it in place with sling sutures. The lateral margins of the recession were approximated with polypropylene sutures and tunnel was closely secured to cover the graft completely. Three months post-treatment showed complete recession coverage, gain in keratinized tissue, increased gingival thickness and complete symptomatic resolution.
Lingual recession in the area of mandibular anterior teeth is a commonly encountered and often ignored clinical scenario. Inflammation caused by calculus, prominent lingual freni and deleterious habits are the most common etiological factors. Gingival augmentation with a minimally invasive technique consisting of an autograft and modified sub periosteal tunnel is presented to address the issues of sensitivity, progressive recession and facilitation of good plaque control.
Gingival recession, Lingual, Tunneling, Sub-epithelial connective tissue, Graft, Sensitivity
SCTG: Sub-Epithelial Connective Tissue Graft; CEJ: Cement-Enamel Junction; TID: Three Times a Day
Gingival recession is defined as the apical shift of the gingival margin with respect to the cemento-enamel junction (CEJ); it is associated with attachment loss and with exposure of the root surface to the oral environment [1]. Potential etiologic factors of gingival recessions are associated with position and anatomy of teeth in the dental arch, osseous dehiscence, alveolar mucosa, thin biotype, excessive or incorrect tooth brushing, muscle pull, or orthodontic treatment [2]. Recession resulting in root surface exposure may affect the esthetic appearance, increase root sensitivity and difficulties in performing adequate oral hygiene measures, consequently facilitating the progression of gingivitis and root caries [1,3].
Different gingival grafting techniques have been utilized for the treatment of mandibular recessions. They include flap designs encompassing envelope, coronally or laterally positioned flap, double pedicle flap, tunneling, or laterally positioned pedicle flap and are often combined sub epithelial connective tissue grafts whereas free gingival graft is used without the need for a flap at the recipient site [4-6]. The above procedures usually require a split thickness flap approach for the various flap designs that may be challenging to execute, especially in the mandibular anterior area. Post-operative complications with the flap procedure may be associated with perforation and/or necrosis of the graft. The modified coronally advanced tunnel (MCAT) was introduced to counter the potential complication, comprising of both combined full and partial-thickness tunnel followed by coronal displacement and held in place with suspension sutures [7]. Nonetheless, it is particularly difficult to achieve tension-free coronal displacement of the tunnel flap in a deep isolated mandibular recession areas and coronal tension can result in loss of vestibule and flap necrosis.
Sculean recently described treatment of deep isolated mandibular recession areas showing successful results at 12 months. Complete root coverage (CRC) was obtained in 17 of the 24 defects, 7 defects root coverage (RC) amounted to 80% to 90% (in 6 cases) and 79% (in 1 case). CRC was found in 6 of the 10 Class III defects. Sculean, et al. described a novel surgical technique, the laterally closed tunnel, specifically intended for deep isolated mandibular Miller Class I, II, and III recessions [8].
However, it is well known clinically that any lingual recession is difficult to manage surgically. This article introduces a simplified protocol of laterally closed tunnel on the lingual surface with sub-epithelial connective tissue graft on an isolated mandibular incisor root.
A 33-year-old male patient was referred to the University Of Tennessee, Graduate Periodontics, with a chief complaint of "irritating painful gums on the lower teeth and a coated sticky texture", confined from #23 to 26 with #23 being most severe. Patient complained sensitivity to hot and cold liquids and a constant discomfort in the area of mandibular anteriors. The patient explained that he was constantly aware of the "changed texture" in this area making it very uncomfortable to the tongue. Medical history was not significant except for Zoloft for anxiety. Habit history included tobacco dip for a period of 6-7 years, quit with nicotine patch and lozenges kept in the mandibular lingual area; a suspected cause for the symptoms of pain and discomfort in the same, since the last 2 years. Dental history was limited to past orthodontic treatment and gingival flap debridement in the mandibular anterior area a year ago at a private office. Previous orthodontic treatment or his previous tobacco habit both, could have been the etiological factors for the lingual recession. Since the patient was already on an orthodontic retainer and recession had progressed, a graft was indicated to not only thicken tissues if further movement was carried out, but to also treat the recession and corresponding symptoms.
A thorough periodontal evaluation revealed generalized probing depths within normal limits and minimal bleeding on probing. The gingiva was pink and firm with thin biotype on maxillary and mandibular anterior teeth. Localized 4 mm lingual recession was noted on #23 with erythematous rolled out gingival margins (Figure 1). Though it is not possible to classify lingual recession according the popular Miller classification, the recession was similar to Miller to Class 2 on the facial with no interproximal bone loss and recession extending up to the mucogingival junction Bitewing and periapical radiographs revealed mild to no horizontal bone loss interdentally.
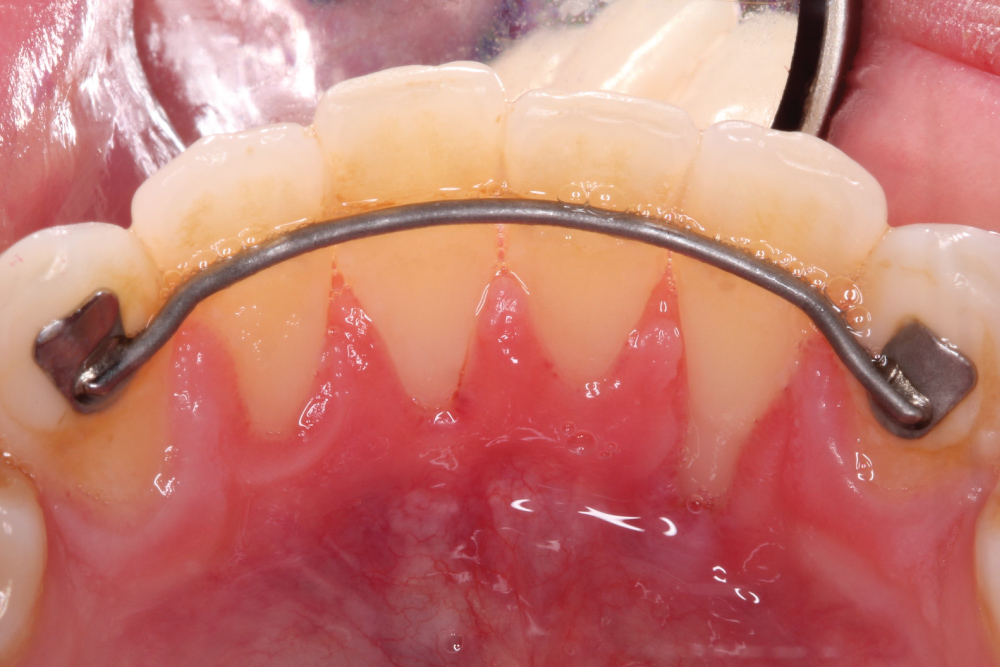 Figure 1: Preoperative view of mandibular anterior lingual area showing deep isolated lingual recession on #23. View Figure 1
Figure 1: Preoperative view of mandibular anterior lingual area showing deep isolated lingual recession on #23. View Figure 1
Findings, treatment options and risks for sub epithelial connective graft on the mandibular lingual region were discussed with patient and consent obtained for the same. Prior to surgery, patient was asked to rinse with 0.2% chlorhexidine digluconate solution. After administering local anesthesia (2% lidocaine with 1/100,000 epi), the exposed root surface was debrided with curettes and piezo tip. Intrasulcular incisions were made on lingual of #22-24 with #15 blade. Instruments included in the Pat Allen soft tissue kit were used to undermine the lingual soft tissue, careful to not perforate the lingual mucosa. The dissection was extended apically beyond mucogingival junction and laterally extending beyond #22-24 sites without severing the intact interdental papilla. Tension free mobility of the soft tissue complex was achieved by carefully reflecting apically, mesially and distally to form a sub-periosteal tunnel or a pouch (Figure 2). Any muscle fibers still present were carefully released. Due to access difficulty, care was taken to prevent any mucosal perforations and release of the interdental papillae. The gingival margin of the recession was passively approximated covering most of the exposed root surface. The exposed root of #23 was burnished with tetracycline and irrigated with saline.
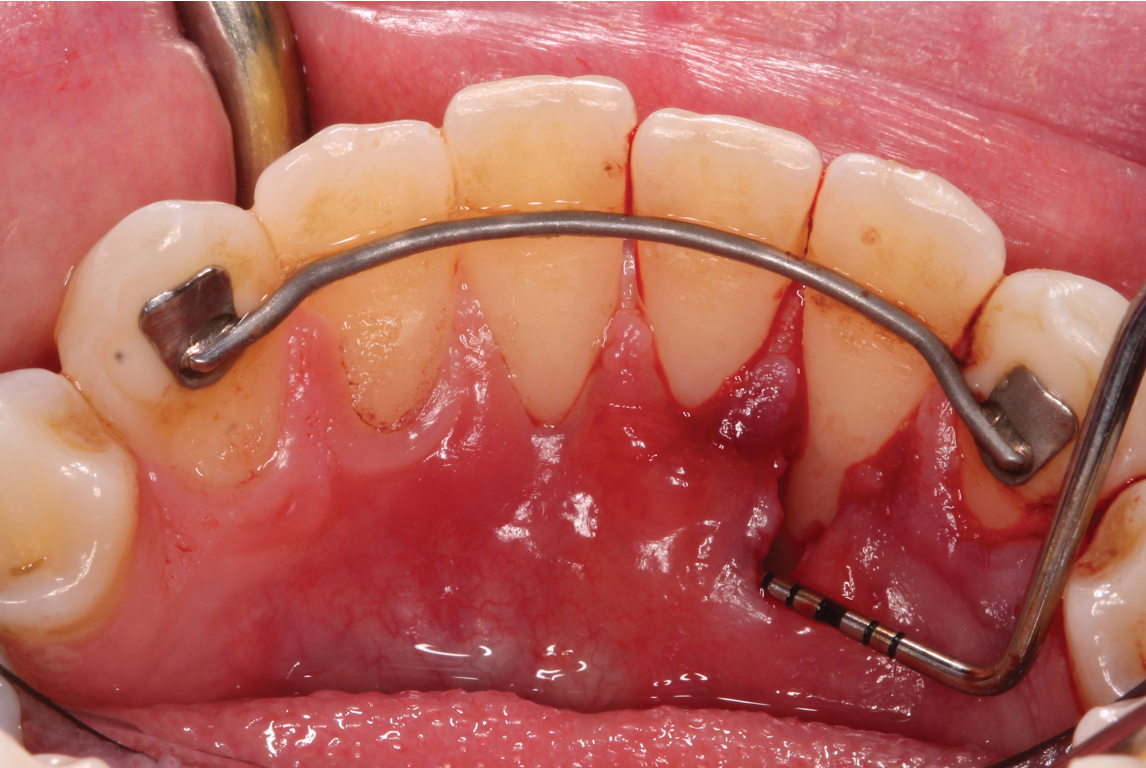 Figure 2: Tension free pouch created to receive the SCTG. View Figure 2
Figure 2: Tension free pouch created to receive the SCTG. View Figure 2
A sub-epithelial connective tissue graft (SCTG) was harvested using double parallel incisions as described by Harris on palate which was approximately 15 mm in length [9] (Figure 3). The donor site was closed by cross mattress stabilizing sutures using 4.0 chromic gut. Stabilizing sling suture was utilized to stabilize the connective tissue graft at the recipient site. The graft was tunneled laterally underneath adjacent papilla. 5.0 chromic sutures were used to sling the graft to #23 (Figure 4). After the SCTG was fixed by the sling sutures to the lingual exposed root surface at the CEJ, lateral margin of recession was approximated to cover the graft and closed with 6.0 polypropylene sutures. Simple interrupted loop sutures were utilized to close margins (Figure 5 and Figure 6). Only a minimal amount of connective tissue graft was exposed after approximating the lateral margins. Hemostasis was achieved with compression by a gauze.
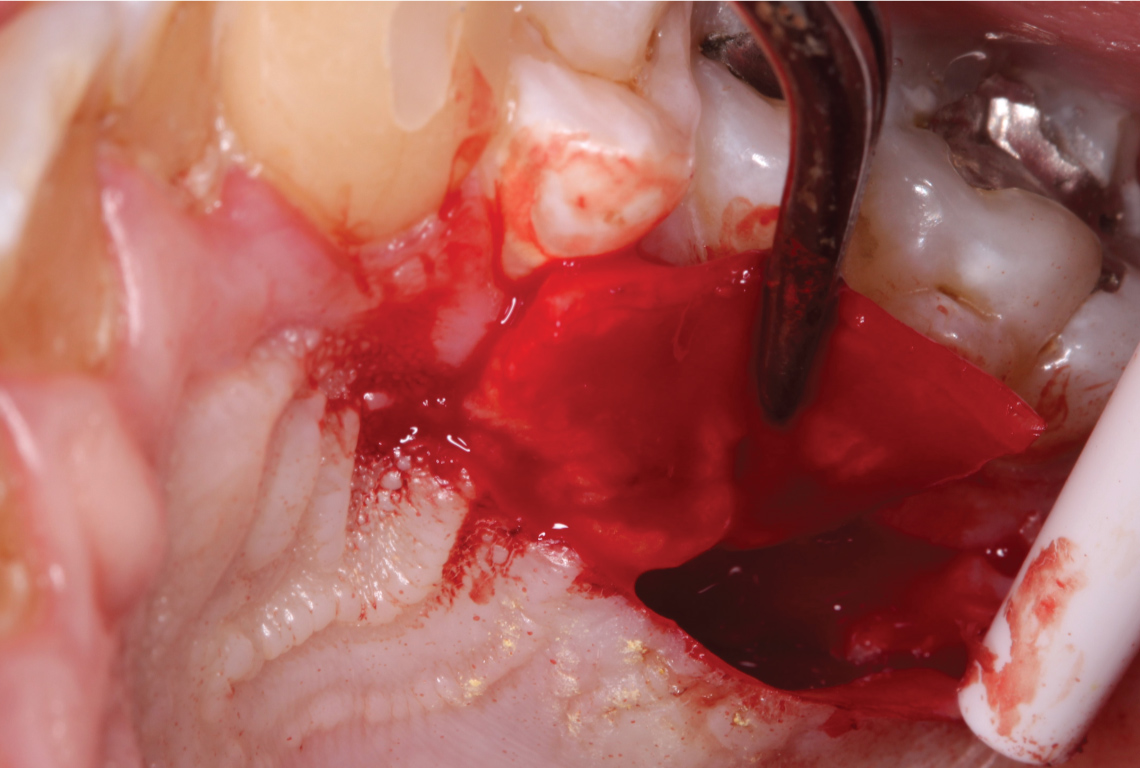 Figure 3: SCTG harvested from the palate with a double incision technique. View Figure 3
Figure 3: SCTG harvested from the palate with a double incision technique. View Figure 3
 Figure 4: The graft was tunneled laterally underneath adjacent papilla with 5.0 chromic gut sutures. View Figure 4
Figure 4: The graft was tunneled laterally underneath adjacent papilla with 5.0 chromic gut sutures. View Figure 4
 Figure 5: SCTG in place against the recession of #23. View Figure 5
Figure 5: SCTG in place against the recession of #23. View Figure 5
 Figure 6: Margins of the sub-periosteal tunnel approximated with 6.0 polypropylene sutures. View Figure 6
Figure 6: Margins of the sub-periosteal tunnel approximated with 6.0 polypropylene sutures. View Figure 6
Postoperatively, the patient was prescribed 500 mg of amoxicillin TID for 7 days to prevent potential infection, 800 mg ibuprofen TID for pain management and twice daily rinse with 0.12% Chlorohexidine rinse for 2 weeks. Patient was instructed to not brush the surgical area for at least 2 weeks. Sutures were removed at 2 weeks after surgery and returned to regular post-operative oral hygiene at 1 month and regular dental recall appointments (Figure 7).
 Figure 7: Post-operative view at 2 weeks. View Figure 7
Figure 7: Post-operative view at 2 weeks. View Figure 7
At 1 month follow up, full coverage of the recession was observed but margin was still erythematous in presentation. Palatal tissue completely epithelialized and patient reported improvement of "gum irritation" on #23 site. The results were stable at a 3 month follow up with 100% lingual root coverage, gingival margin to the CEJ, gingival tissue firm and color consistent with the adjacent tissue color (Figure 8). The patient was very satisfied with the procedure as his primary complaint of pain and discomfort at the site was addressed.
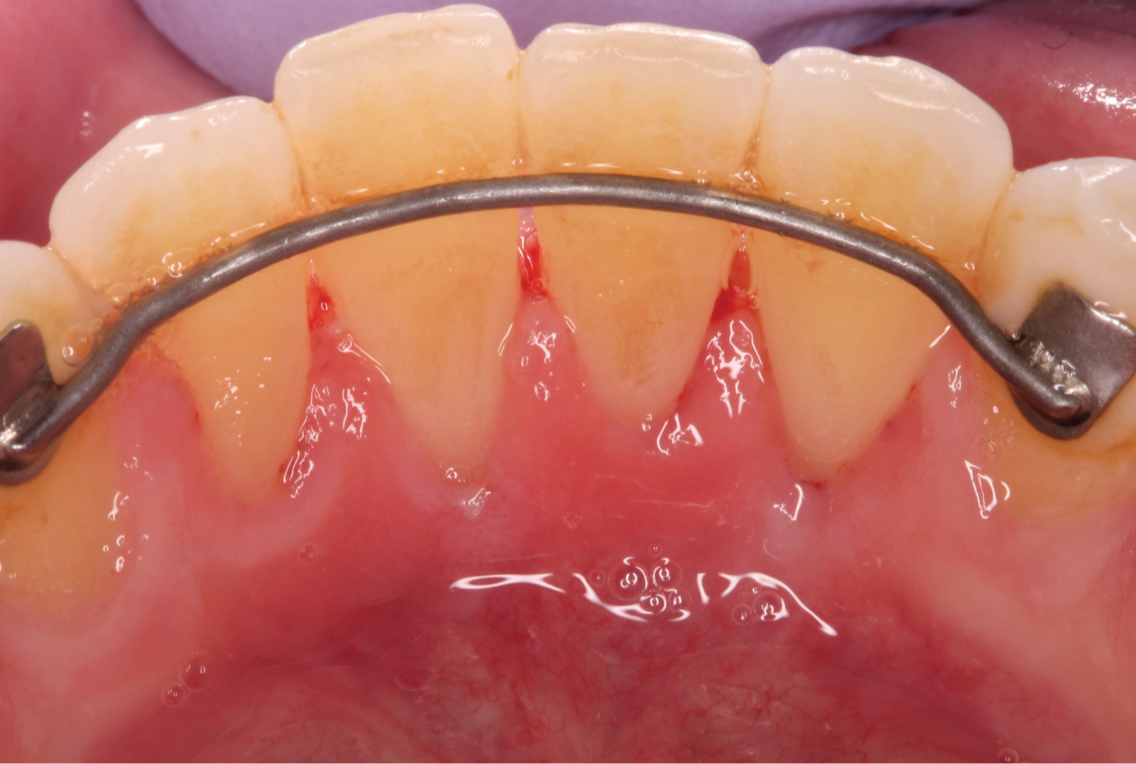 Figure 8: Post-operative view at 3 months. View Figure 8
Figure 8: Post-operative view at 3 months. View Figure 8
A variety of techniques and materials have become popular to treat gingival recession since the original SCTG procedure proposed by Langer and Langer, but SCTG is still considered to be the gold standard due to its predictability in achieving root coverage [10]. SCTG-based procedures have showed most stable long term outcomes with respect to recession coverage, gain in keratinized tissue and compete root coverage [11]. Though these results have been well documented in Millers Class 1 or 2 recession defects especially on the labial and buccal surfaces, there has been very limited literature on treatment of lingual recession defect. Lingual recession cannot be classified by Miller classification hence a modern classification by Cairo, based on the interdental CAL is used for our clinical presentation and will fall in "Recession Type 1 (RT1)". This includes gingival recession with no interproximal attachment loss and interproximal CEJ clinically not detectable on both mesial and distal [12].
Though lingual recession is fairly common in mandibular anterior region due to the propensity of calculus accumulation in this region and subsequent gingival inflammation and bone loss, treatment of mandibular lingual areas is surprisingly not attempted routinely. The anatomical challenges due to the thin and mobile lingual mucosa, muscle attachments and the surgical difficulty of raising a lingual flap in addition to lack of esthetic concern presents a unique scenario often bordering on watchful neglect. However, in rare situations when the patient is symptomatic as a result of the recession, the wait and watch attitude calls for surgical intervention.
Due to challenging surgical site the most predictable treatment methodology of SCTG was selected. SCTG is shown to be the treatment of choice most often selected when dentinal hypersensitivity was a concern and is was important to prevent further recession and root caries. The American academy of periodontology regenerative workshop came to a consensus that SCTG shows the best clinical outcomes for root coverage procedures as regards mean and complete root coverage and gain in keratinized tissue for Millers Class 1 and 2 recession defects [3].
The tunneling flap technique has its origins from the envelope flap by Raetzke [13], wherein he avoided vertical releasing incisions resulting in a more simplified procedure and better esthetic and healing outcomes. Zabalegui [14], the creator of tunneling technique connected multiple envelopes to form the sub-periosteal tunnel whereas Azzi [15] released the interdental papilla to mobilize the tunnel flap and cover the recession defect. Sculean’s modification of the tunnel was to suture the lateral margins of isolated labial recession defects [8]. These techniques gained popularity for labial and buccal areas, however there is limited evidence for treatment of lingual areas. Our case uniquely shows successful results on the surgically challenging mandibular lingual areas, a demanding and technique sensitive site to achieve a tension free, perforation free tunnel that can be displaced coronally. Elevation of the interdental papilla was performed to achieve mobility necessary for coronal displacement and the recession margins were approximated to cover the SCTG as it is harder to achieve complete coronal displacement in single recession defects greater than 3 mm by coronal displacement alone. Microsurgical suturing with fine needles and suture materials and small amounts of exposed connective tissue are helpful in achieving a harmonious gingival margin.
The present case report indicates that it is possible to successfully and predictably treat isolated lingual recession defects with a laterally closed tunneling technique and that the connective tissue graft still dominates effective method to cover exposed roots.