Pelvic hematomas can be a serious complication of vaginal delivery. They can be associated with significant morbidity related to blood loss, infection, surgery and blood product transfusion. Reported incidence varies from 1/300 to 1/1500 [1]. Operative vaginal delivery and episiotomy are among the most common risk factors associated with puerperal hematomas, but they may also occur in the absence of laceration of the surrounding tissue [1,2]. They are classified as vulvar, vaginal, vulvovaginal or retroperitoneal. The majority of puerperal hematomas are vulvovaginal and can involve either branches of the pudendal artery or the descending branch of the uterine artery [3]. However, the haemorrhage can also be of venous origin since the veins of the perineum are valveless and have free anastomoses with large intrapelvic venous plexuses [2,4]. Most hematomas will present within 24 hours of delivery. Perineal pain and pressure are common presenting symptoms along with a palpable tender mass [5].
Management of puerperal hematomas is controversial. Conservative management, surgical intervention and selective arterial embolization are the three main methods for managing puerperal hematomas. Conservative management consists of pressure packing, ice packs, analgesia and close surveillance [6]. Surgical intervention is indicated in cases of acute expansion, large hematomas or unsuccessful conservative management. It includes incision, evacuation of clots and ligation of the bleeding if identified, although in many cases, the lacerated vessel cannot be identified since the bleeding is venous in nature and from multiple sites. A layered closure should be performed to secure hemostasis. A vaginal pack or a balloon tamponade can be left in place for 12 to 24 hours. When mainstay methods of suture and packing fail or when arterial bleeding is identified, transcatheter arterial embolization becomes an interesting alternative [1,3].
We report a case of refractive puerperal hematoma, treated with coil embolization.
A 32-year-old female, G3P1A1, with a past medical history of C-section, gave birth vaginally to a healthy term infant weighing 3530 g. Delivery was free of any immediate complication, except for some superficial vulvar abrasions. No episiotomy was performed.
A few hours after delivery, she complained of severe vaginal pain and tenesmus. Physical examination revealed a 6 cm × 6 cm right vaginal hematoma. The hematoma was surgically evacuated under general anesthesia soon after diagnosis. Treatment was completed by vaginal suturing and packing. Hemostasis was achieved.
The next day, hemoglobin level, which was normal upon her arrival at the delivery room, dropped to 73 g/L. She received 2 blood transfusions and was initially stable. Bleeding resumed on the following day and suspected recurrence of the vaginal hematoma was confirmed by physical examination. She underwent a second surgical drainage of the hematoma. However, despite careful exploration, no source of active bleeding was identified.
In the following hours, the patient showed clinical deterioration with an episode of spontaneous vaginal blood clots evacuation, estimated to 1000 mL, and increasing pain. Her hemoglobin continued to drop, requiring multiple transfusions.
Confronted to this unstable clinical picture, a CT-angiogram of the pelvis was performed, showing a 11 cm × 6 cm × 14 cm right paravaginal hematoma (Figure 1). The arterial phase showed a round 16 mm × 18 mm pseudoaneurysm at the inferior margin of the hematoma, originating from a distal branch of the internal pudendal artery (Figure 2).
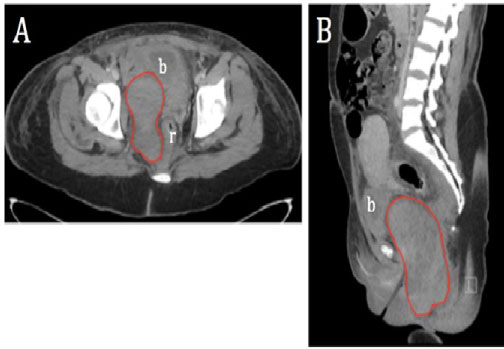 Figure 1: Venous phase contrast-enhanced computed tomography. A) Axial; B) Sagittal images show a large right pelvic hematoma (red outline), surrounded by a hemorrhagic suffusion extending superiorly in the space of Retzius and inferiorly in the ischio-rectal fossa and perineal pouch. Bladder (b) and rectum (r) are displaced to the left by the hematoma.
View Figure 1
Figure 1: Venous phase contrast-enhanced computed tomography. A) Axial; B) Sagittal images show a large right pelvic hematoma (red outline), surrounded by a hemorrhagic suffusion extending superiorly in the space of Retzius and inferiorly in the ischio-rectal fossa and perineal pouch. Bladder (b) and rectum (r) are displaced to the left by the hematoma.
View Figure 1
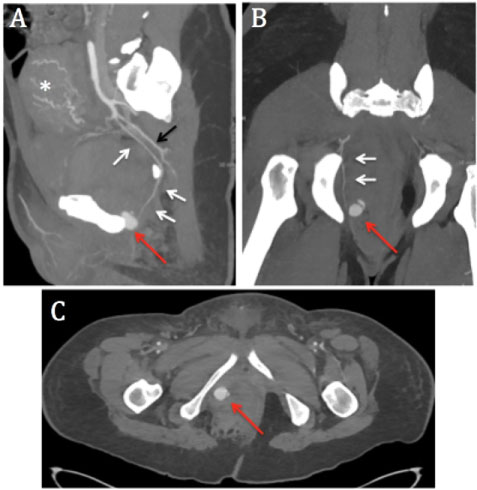 Figure 2: Arterial phase contrast-enhanced computed tomography. A) Sagittal; B) Coronal; C) Axial maximum intensity projection (MIP) images show a distal right internal pudendal artery pseudoaneurysm (red arrow). White arrows indicate the right pudendal artery originating from the anterior division of the internal iliac artery and exiting the pelvis through the greater sciatic foramen, curving around the ischial spine and re-entering the pelvis through the lesser sciatic foramen. Pudendal artery lies anteriorly to the inferior gluteal artery (black arrow). Dilated uterine arteries (asterisk) are also seen, in relation with early post-partum state.
View Figure 2
Figure 2: Arterial phase contrast-enhanced computed tomography. A) Sagittal; B) Coronal; C) Axial maximum intensity projection (MIP) images show a distal right internal pudendal artery pseudoaneurysm (red arrow). White arrows indicate the right pudendal artery originating from the anterior division of the internal iliac artery and exiting the pelvis through the greater sciatic foramen, curving around the ischial spine and re-entering the pelvis through the lesser sciatic foramen. Pudendal artery lies anteriorly to the inferior gluteal artery (black arrow). Dilated uterine arteries (asterisk) are also seen, in relation with early post-partum state.
View Figure 2
The patient subsequently underwent angiography in the next hour, which confirmed the findings described on the previous CT-scan (Figure 3). The right internal pudendal artery pseudoaneurysm was embolized with multiple coils (Figure 4).
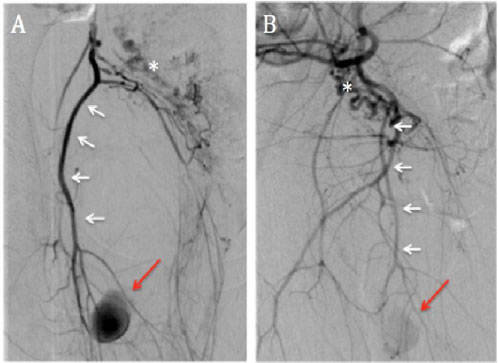 Figure 3: Distal right internal iliac artery angiography. Subtracted right anterior oblique A) And left anterior oblique; B) Acquisitions, before embolization, show a pseudoaneurysm arising from a distal branch of the right internal pudendal artery (red arrow). White arrows indicate the internal pudendal artery. Dilated uterine arteries (asterisks) are displaced to the left by the pelvic hematoma.
View Figure 3
Figure 3: Distal right internal iliac artery angiography. Subtracted right anterior oblique A) And left anterior oblique; B) Acquisitions, before embolization, show a pseudoaneurysm arising from a distal branch of the right internal pudendal artery (red arrow). White arrows indicate the internal pudendal artery. Dilated uterine arteries (asterisks) are displaced to the left by the pelvic hematoma.
View Figure 3
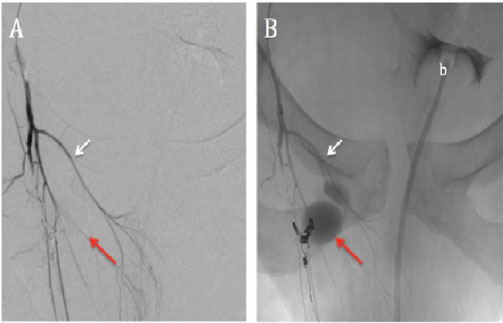 Figure 4: Selective right internal pudendal artery angiography. A) Subtracted; B) Unsubtracted right anterior oblique acquisitions, after coil embolization, show complete exclusion of the pseudoaneurysm with contrast stagnation (red arrow). Five 2 and 3-mm detachable coils were deployed in the efferent vessel, neck and afferent vessel of the pseudoaneurysm (sandwich technique). Images also show some of the terminal branches of the right internal pudendal artery, including the inferior rectal artery (white arrows). Bladder and urinary catheter (b) are displaced to the left by the pelvic hematoma.
View Figure 4
Figure 4: Selective right internal pudendal artery angiography. A) Subtracted; B) Unsubtracted right anterior oblique acquisitions, after coil embolization, show complete exclusion of the pseudoaneurysm with contrast stagnation (red arrow). Five 2 and 3-mm detachable coils were deployed in the efferent vessel, neck and afferent vessel of the pseudoaneurysm (sandwich technique). Images also show some of the terminal branches of the right internal pudendal artery, including the inferior rectal artery (white arrows). Bladder and urinary catheter (b) are displaced to the left by the pelvic hematoma.
View Figure 4
The patient's medical condition improved rapidly over the next few days. Her hemoglobin level stabilized and the pain eventually resolved. She was discharged 3 days after the angiographic procedure, without any other complications.
Selective arterial embolization of uterine arteries is already a widely accepted treatment option in the management of postpartum hemorrhage of uterine origin, especially in uterine atony, when conservative measures have failed. It is effective, with a technical success of 70-90% and safe, with a complication rate of less than 5%. Since non-permanent embolic agents are used, it is considered a fertility-preserving procedure [7]. In fact, many studies on uterine embolization in the treatment of postpartum haemorrhage concluded that menstruations and fertility were not affected [8-11].
In selected cases, it has successfully replaced uterus-preserving surgical procedures like uterine compression sutures and vascular ligation.
Arterial embolization is also a promising alternative in the treatment of postpartum hemorrhage related to lower genital tract injury, when initial surgical treatment fails. The first successful case of embolization was reported in 1979 by Brown, et al. [12], when bilateral surgical internal iliac artery ligation and hysterectomy had previously failed to control the bleeding. Although arterial embolization in the treatment of postpartum vulvovaginal haemorrhage is now increasingly reported in case series, there is neither strong evidence nor established guidelines on the subject in the literature.
A recent review of 60 patients, currently the largest series in literature, reported a technical and clinical success rate of 98% and 88%, respectively [13]. The procedure is safe, with few minor complications reported, like fever and leg oedema [13]. No vulvo-vaginal wall necrosis has been observed, even in cases where permanent embolic agents were used. The very rare cases of amenorrhea reported in this study were not attributable to the embolization itself, according to the authors [13].
Gelfoam was the embolic agent of choice in most studies. Other permanent embolic agents like n-butyl cyanoacrylate (NBCA) glue, microcoils and polyvinyl alcohol particles (PVA) have also been used [13-15]. The choice of embolic agent depends on the type and size of the bleeding focus, on the feasibility of selective catheterization of the target vessel and ultimately, on the operator's preference.
A multiphase abdominal and pelvic CT, with unenhanced, arterial and venous phases, should always be obtained prior to angiography to confirm the arterial nature of the bleeding and identify the bleeding vessel, in order to plan the procedure. Vaginal, internal pudendal and cervico-vaginal branches of the uterine artery, which are all branches of the anterior division of the internal iliac artery, represent the most frequently embolized vessels. If no active extravasation or pseudoaneurysm is identified on internal iliac artery angiography, bleeding from other vessels such as the inferior mesenteric and the external pudendal arteries should be suspected [13].
In conclusion, pudendal artery pseudoaneurysm is an uncommon cause of puerperal hemorrhage and pelvic hematoma. Transcatheter arterial embolization, which is now a widely accepted treatment option for postpartum uterine hemorrhage, also seems safe and effective for the management of hemorrhage related to lower genital tract injury. Patients with large postpartum pelvic hematomas or recurrent post-partum hemorrhage related to lower genital tract injury should undergo angio-CT and embolization if an arterial bleeding is identified.