The basilar artery is the main arterial contributor to the posterior circulation. Interruptions of this flow can cause devastating strokes and neurological demise. While most patients with a basilar artery occlusion suffer from a high rate or morbidity and/or mortality, a small subset survive but have progressive symptomatic decline. Delayed revascularization of these patients with chronic basilar artery occlusions based on symptomatic progression may provide a favorable risk-benefit ratio, but requires appropriate patient selection.
Basilar artery occlusion, Ischemic stroke, Revascularization
The basilar artery is the main contributor to arterial perfusion for the posterior circulation, including the brainstem, cerebellum, thalami, occipital lobes, and medial temporal lobes [1,2]. Unsurprisingly, acute untreated interruptions in blood flow to these areas due to basilar artery occlusion (BAO) result in a high rate of morbidity and mortality if not recanalized [2-5]. However, a small subset patients survive the acute stage but can progress, continuing to suffer symptoms and ultimately strokes due to chronic BAO [6,7].
Cardiac literature has shown some promising results in the management of chronic occlusions with revascularization [8]. While previous attempts at revascularization via extracranial circulation-intracranial circulation (EC-IC) bypass have been plagued by high complication rates [1], promising results have been reported via endovascular approach for the management of chronic BAO [2,9].
A 67-year-old female with a baseline modified Rankin score of 0 presented after a transient episode of dysarthria and right facial paresthesias. She was on aspirin for a history of small stroke one year prior in the left parietal lobe, without any residual deficit. Platelet function assay (PFA) using epinephrine showed she was therapeutic when on aspirin therapy; this assay allows for evaluation of platelet function during a simulated vascular injury in-vitro. She was found to have severe stenosis of the basilar artery (Figure 1A) but remained asymptomatic. She was placed on dual antiplatelet therapy with aspirin 81 mg daily and ticagrelor 60 mg twice daily, and P2Y12 receptor reactivity - a test of the ability of activated platelets to find fibrinogen - was therapeutic.
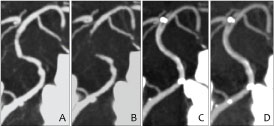 Figure 1: CT angiography of the basilar artery before and after treatment. A) CT angiogram showing atherosclerosis of the basilar artery 1 year prior to treatment; B) Complete occlusion of basilar artery noted 4 days prior to treatment. Imaging of the basilar artery 1 day; C) And 11 months; D) After angioplasty and stenting demonstrate patency of the stent. View Figure 1
Figure 1: CT angiography of the basilar artery before and after treatment. A) CT angiogram showing atherosclerosis of the basilar artery 1 year prior to treatment; B) Complete occlusion of basilar artery noted 4 days prior to treatment. Imaging of the basilar artery 1 day; C) And 11 months; D) After angioplasty and stenting demonstrate patency of the stent. View Figure 1
She returned to the hospital two months later with complaint of generalized malaise for several weeks. Repeat computer tomography (CT) angiogram was obtained, revealing a basilar artery occlusion that had progressed since her initial presentation (Figure 1B), despite her strict adherence to medical therapy as confirmed by continually therapeutic P2Y12 receptor reactivity assays - of note she was not on any medication that would confound these test results. This imaging finding was confirmed with catheter angiogram. Magnetic resonance imaging (MRI) showed punctate strokes in the cerebral peduncle and pons (Figure 2A). Given the angiographic nature of the complete occlusion and the stability of her symptoms, decision was made to continue dual antiplatelet therapy and close follow-up after lengthy discussion with the patient, without emergent endovascular intervention.
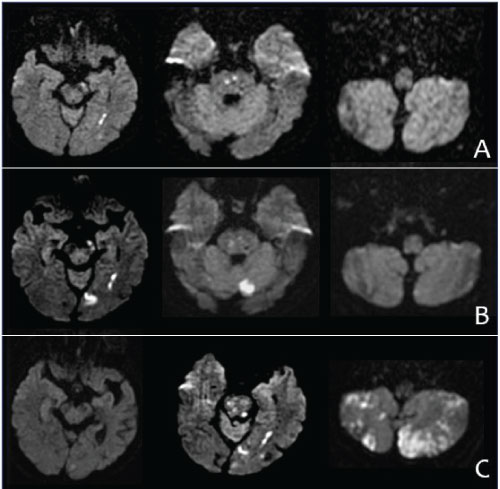 Figure 2: Evolution of strokes before and after stenting and angioplasty of basilar artery occlusion. A) MRI 4 days prior to stenting reveals stroke in the left cerebral peduncle and pons; B) The patient had a second stroke in the occipital lobe immediately prior to stenting; C) The patient had some increased speech difficulty and right sided weakness/dysmetria following stenting of the basilar artery occlusion. Symptoms were attributed to bilateral strokes in the cerebellum and pons. View Figure 2
Figure 2: Evolution of strokes before and after stenting and angioplasty of basilar artery occlusion. A) MRI 4 days prior to stenting reveals stroke in the left cerebral peduncle and pons; B) The patient had a second stroke in the occipital lobe immediately prior to stenting; C) The patient had some increased speech difficulty and right sided weakness/dysmetria following stenting of the basilar artery occlusion. Symptoms were attributed to bilateral strokes in the cerebellum and pons. View Figure 2
Four days later she presented with complaint of visual changes, slurred speech, and lower extremity weakness. An MRI revealed a new left occipital stroke (Figure 2B). Since the patient was still having frequent strokes on maximal medical management, stenting and angioplasty of the basilar artery was offered. Risks include - but are not limited to - intracranial hemorrhage from reperfusion injury or vessel perforation, vessel dissection, stroke from occlusion of a perforating artery, embolic shower causing distal stroke, transient or permanent neurological deficits, cardiac event such as myocardial infarction, and renal injury. More serious adverse events such as coma or death are also discussed with patients and their families.
The procedure was performed under general anesthesia. Primary access was obtained via the right common femoral artery. An 80 cm Cook Shuttle Sheath (Cook Medical) was navigated into the innominate artery over a 125 cm 6 French Simm-2 selection catheter (Cook, special order) and 0.035" Stiff Shaft Glidewire (Terumo). A 5 French 115 cm Navien intermediate guide catheter (Medtronic) was then navigated into the distal cervical vertebral artery over a 0.035" Standard Shaft Glidewire (Terumo). A catheter angiogram from the right vertebral artery confirmed that there was no antegrade flow (Figure 3B). We then attempted to cross the occluded basilar artery with a Headway 17 microcatheter (Microvention) over a Synchro-2 soft microwire (Stryker), but felt the wire was taking a more tortuous course than anticipated. In order pass the occlusion more safely, we performed the following two actions:
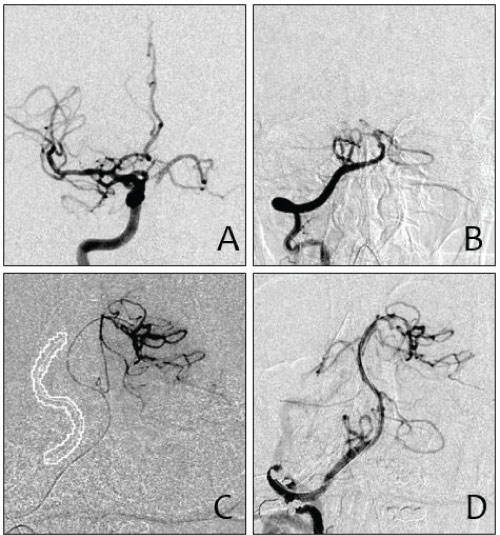 Figure 3: Pre-treatment angiograms from the carotid. A) And vertebral artery; B) Demonstrate complete occlusion of the mid-segment of the basilar artery; C) A 3-D roadmap by fusing 1-year-old CTA obtained when the basilar artery was still patent to the current 3D catheter angiogram to help cross the lesion; D) Basilar artery is patent after angioplasty and deployment of an Enterprise stent. View Figure 3
Figure 3: Pre-treatment angiograms from the carotid. A) And vertebral artery; B) Demonstrate complete occlusion of the mid-segment of the basilar artery; C) A 3-D roadmap by fusing 1-year-old CTA obtained when the basilar artery was still patent to the current 3D catheter angiogram to help cross the lesion; D) Basilar artery is patent after angioplasty and deployment of an Enterprise stent. View Figure 3
1. In order to see the posterior cerebral artery (PCA) and basilar apex better, we decided to place a 5 French diagnostic catheter into the right internal carotid artery (ICA) through a secondary access point in the left common femoral artery (Figure 3A).
2. We performed a non-contrast enhanced 20 second dynamic computed tomograph (DCT) at 109 kv and fused the images to a prior CT angiogram in which the basilar artery was still patent to use as a 3D roadmap (Figure 3C).
Using 3D roadmap, we were able pass the catheter through the occluded segment of the basilar artery and into the left PCA and perform a microcatheter run. The Synchro-2 soft wire was then exchanged for a 300 cm 0.014" MIRACLEbros 6 microwire. Multiple angioplasties were performed of the entire occluded segment with a 1.5 mm × 15 mm Maverick over the wire balloon (Boston Scientific). A Prowler Select Plus 021" microcatheter was then readvanced over the MIRACLEbros microwire into the left PCA and a used to deploy a 4 mm × 39 mm Enterprise 2 stent across the basilar artery. A post-stent angioplasty was then performed using a 2.25 mm × 15 mm Gateway balloon (Boston Scientific) over a Synchro-2 soft wire (Figure 3D). The Enterprise stent was chosen because it has similar physical properties to the Wingspan stent but was available in a length long enough to cover the entire lesion with one device.
The patient had some increased speech difficulty, right sided weakness, and dysmetria following stenting of the basilar artery occlusion. Symptoms were attributed to bilateral strokes in the cerebellum and pons (Figure 2C). Fortunately, she made an excellent recovery in the next 4 weeks including normal speech, upper extremity function, and the ability to walk in a walker. Repeat imaging studies showed continued patency of the basilar artery (Figure 1C and Figure 1D). She had some residual gait difficulty one year out, but was able to return to functional independence, with a modified Rankin score of 1. She remained on dual antiplatelet therapy, taking aspirin 81 mg daily and ticagrelor 60 mg twice daily for 6 months, after which she was maintained on aspirin 81 mg daily alone.
For patients with progressive symptoms due to chronic BAO, management options are limited to medical management, surgical bypass, and delayed endovascular revascularization. Medical management is often inadequate in preventing symptomatic progression and infarction due to vertebrobasilar insufficiency, as collaterals are often an insufficient source of perfusion for the posterior circulation [6]. EC-IC bypass via superficial temporal artery to superior cerebellar artery or other posterior circulation bypasses are fraught with high complication rates [1].
Fortunately, improvements in neuroendovascular techniques provide new management options for these patients. The revascularization of chronic BAO carries significant risk and is rarely reported [2,6]. Subacute to chronic revascularization attempts - with a reported delay of up to 8 months from angiographic confirmation of an occlusion, and even longer from symptomatic onset - have shown an improvement compared to previous management strategies despite the high rate of complications [6,7].
Protection against ischemic events during intracranial angioplasty and stenting remains challenging. Post-procedure DWI lesions are common after intracranial stenting and angioplasty procedures and are caused by a combination of emboli and perforator occlusion. Currently, there are no distal protection devices specifically for use in the intracranial circulation. The use of suction catheters for embolic protection have been suggested to prevent distal emboli [10]. The prevention of perforator strokes is theoretically even more challenging and may, to some extent, be unavoidable. It has been suggested that sub-maximal balloon dilation of the lesion a few weeks before stenting may cause fibrosis and stabilization of the plaque and reduce the risk of “snow plowing" it over the adjacent perforating vessels [11].
As mechanical thrombectomy continues to grow as the gold-standard for acute ischemic stroke [12] the management paradigm for chronic malperfusion states continues to evolve. Medical management is often insufficient for heavily symptomatic patients, and EC-IC bypass is a limited option with high complication rates. Although risky, endovascular revascularization at the chronic stage is an attractive option for symptomatic chronic occlusions of the basilar artery.