Primary thyroid gland lymphoma is a rare condition, accounting for only 2% of extranodal lymphomas, usually occurring in patients with autoimmune thyroiditis. Among these lymphomas, B-cell non-Hodgkin lymphoma is the most frequently encountered, while Hodgkin's disease and T-cell lymphomas are extremely rare.
Through this paper, we report 5 primary thyroid lymphoma cases, diagnosed in our department in a period of 6 years (Jan 2012 to Dec 2017), all of them were B-cell Non-Hodgkin Lymphomas.
Primary thyroid lymphoma, Thyroiditis
Primary thyroid lymphoma is very uncommon, representing about 5% of all thyroid malignancies, its clinical presentation is not specific for lymphoma and its diagnosis is very complex, and shouldn't be confirmed after surgery. Despite its rarity, physicians should keep the diagnosis in mind since its management is very different from that of other neoplasms of thyroid gland.
Through this paper, we reviewed all cases (five) of primary thyroid lymphoma diagnosed in our department in a period of 6 years, detailing the clinical findings, management and follow up of our patients, while discussing recent literature in the matter.
We reviewed all five cases of primary thyroid lymphoma diagnosed in the otolaryngology department of Mohammed 6th teaching hospital in Marrakech, Morocco, in a period of 6 years (from January 2012 to December 2017), and treated in both hematology and otolaryngology departments of our university hospital. 4 male and 1 female patients with a median age of 57, with no relevant past medical history except one female patient treated for Hashimoto thyroiditis for 7 years in the endocrinology department, and one male with type 2 diabetes, All the patients were admitted via emergencies presenting a rapidly progressing cervical mass with signs of compression (inspiratory dyspnea, dysphagia and dysphonia), the clinical examination showed noted a voluminous fixed goiter with multiple cervical nodes, two patients had superior vena cava syndrome (Figure 1) and one of them had a Claude Bernard Horner triad (ptosis, myosis and enophtalmy) (Figure 2). Nasofibroscopy showed a unilateral recurrent nerve paralysis in all cases. Patients were admitted to the ICU unit with a where they were stabilized with oxygenotherapy and IV steroids were started. No patient required emergency tracheotomy. The patients then underwent an enhanced CT scan that showed a voluminous cervical mass with vascular and aero-digestive compression (Figure 3). The patients with superior vena cava syndrome and the Claude Bernard Horner triad had an upper mediastinal invasion with mediastinal nodes. Blood tests showed a normal TSH and thyroid hormone levels with elevated inflammatory markers and lactate dehydrogenase levels. Due to the locally advanced stages of the cervical masses, an open biopsy was performed, revealing a Large B-cell Non-Hodgkin lymphoma in all cases (Figure 4 and Figure 5).
 Figure 1: Patient presenting a cervico-mediastinal mass with superior vena cava syndrome with orbital edema, white arrow showing collateral venous circulation.
View Figure 1
Figure 1: Patient presenting a cervico-mediastinal mass with superior vena cava syndrome with orbital edema, white arrow showing collateral venous circulation.
View Figure 1
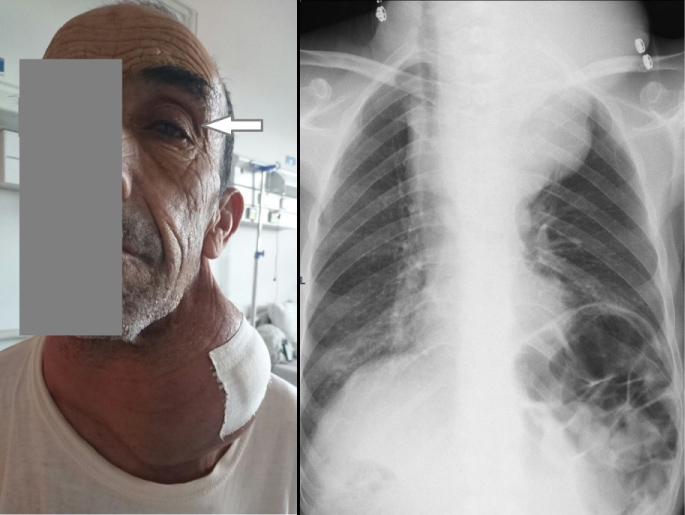 Figure 2: a) Patient presenting a voluminous cervical mass associated with Claude Bernard Horner triad (note the ptosis: white arrow); b) Chest X-ray of the same patient showing a voluminous compressive cervico-mediastinal mass.
View Figure 2
Figure 2: a) Patient presenting a voluminous cervical mass associated with Claude Bernard Horner triad (note the ptosis: white arrow); b) Chest X-ray of the same patient showing a voluminous compressive cervico-mediastinal mass.
View Figure 2
 Figure 3: CT scan in axial and frontal reconstruction showing a voluminous and compressive goiter in a patient presenting a thyroid.
View Figure 3
Figure 3: CT scan in axial and frontal reconstruction showing a voluminous and compressive goiter in a patient presenting a thyroid.
View Figure 3
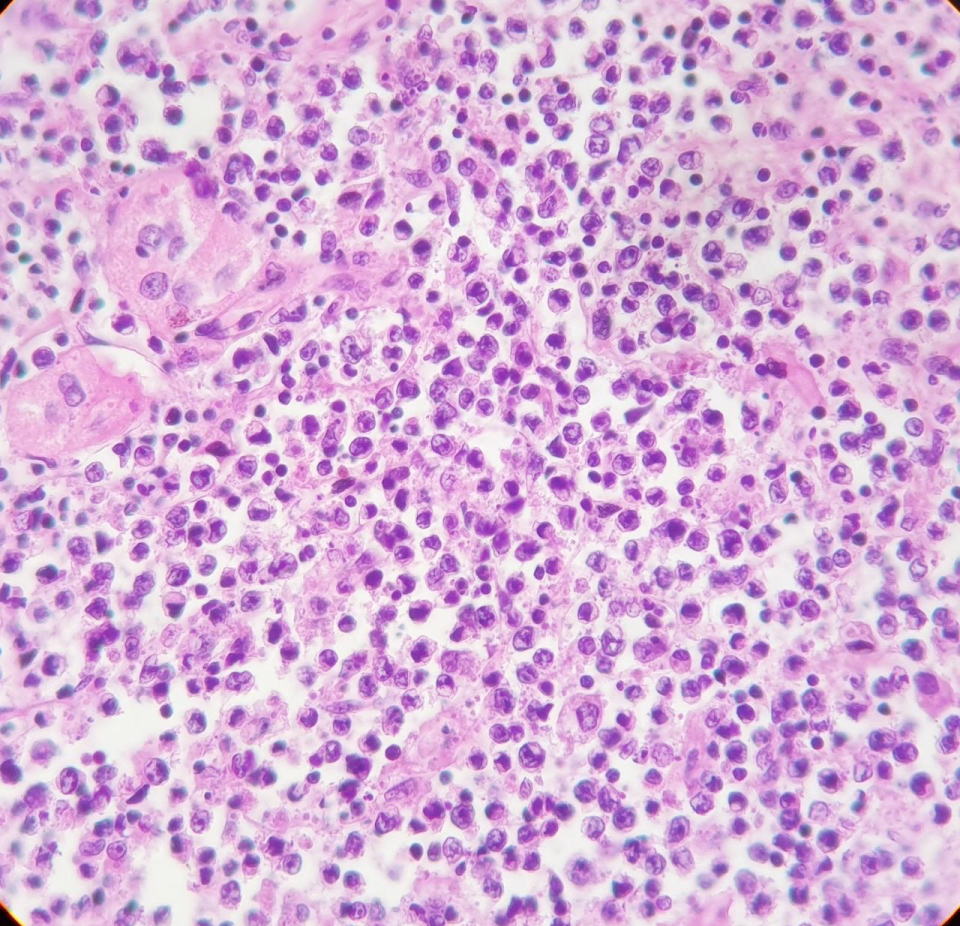 Figure 4: Large lymphomatous cells, high nucleocytoplasmic ratio, anisokaryotic nucleus with prominent nucleolus and mitotic figures.
View Figure 4
Figure 4: Large lymphomatous cells, high nucleocytoplasmic ratio, anisokaryotic nucleus with prominent nucleolus and mitotic figures.
View Figure 4
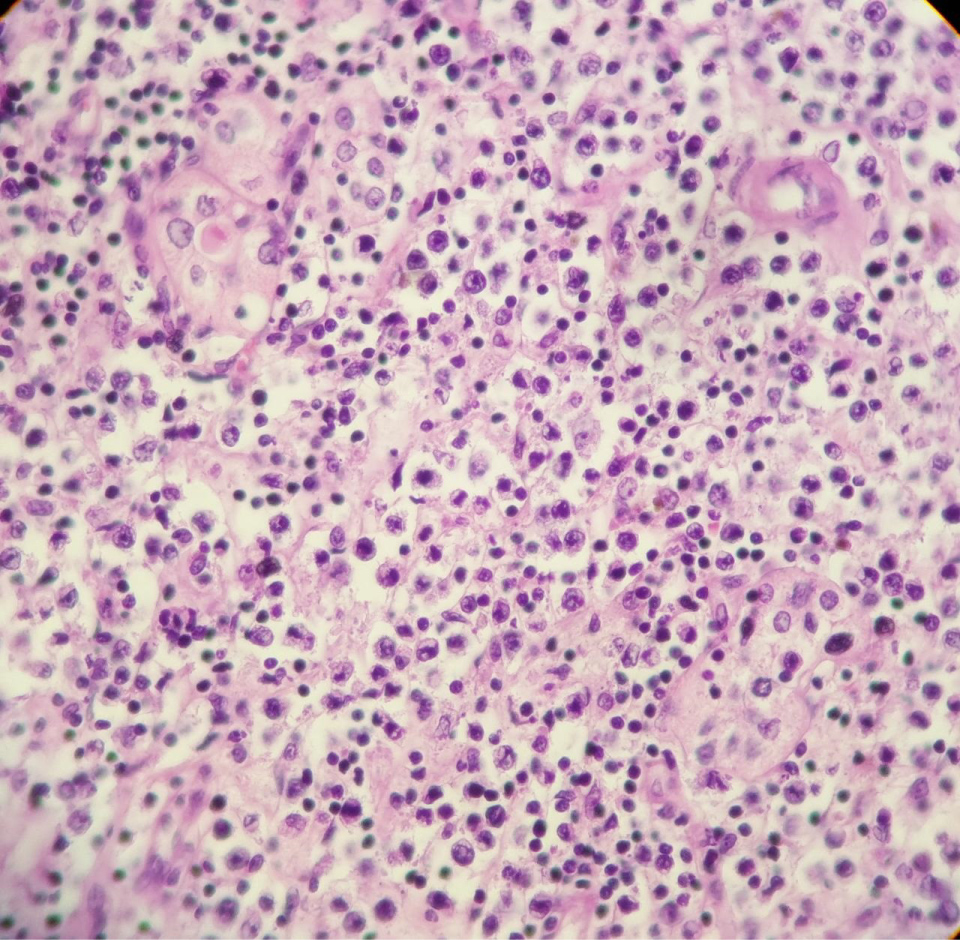 Figure 5: Thyroid localization of a diffuse large cell lymphoma proliferation (hematein-eosin, magnification × 10).
View Figure 5
Figure 5: Thyroid localization of a diffuse large cell lymphoma proliferation (hematein-eosin, magnification × 10).
View Figure 5
A full clinical checkup, lab tests, full body CT-scan and bone marrow biopsy didn't show other locations of the disease except for cervical and mediastinal lymph nodes (Ann Arbor IE in 2 cases and IIE in 3 cases). The patients were then referred to the hematology department where a chemotherapy (R-CHOP) protocol was initiated. One of the patients presenting the superior vena cava syndrome died in the first chemotherapy session, and a second one died 6 months after the treatment started. One patient is still undergoing his chemotherapy (1 year since diagnosis), and the two others patients (IE Ann Arbor) are showing the signs of remission after 18 months and 24 months of follow up.
Most physicians assume that an Eu-TiRADS 5 thyroid mass is most likely to be a tumor arising from thyroid cells. It is usually the case in over 90% of cases. However, it is very important to consider a wider range of differential diagnosis. Among these differentials, primary or secondary lymphomas are to keep in mind. Secondary thyroid metastasis of lymphomas are sometimes encountered, but primary thyroid lymphomas are rarely described, they account for 2% of extranodal lymphomas, and for them to be recognized as such, the impairment must only affect the thyroid gland and eventually, the locoregional lymph nodes, so other primary locations must be ruled out [1].
In primary thyroid lymphomas, B-cell non-Hodgkin lymphomas are the most frequent, while T cell lymphomas and Hodgkin's disease are unusual. Normally, the thyroid gland does not contain lymphoid tissue, this tissue develops under pathological conditions, mainly in autoimmune thyroiditis, probably as a result of chronic antigenic stimulation, and this is why it is very frequent is patients with Hashimoto's thyroiditis (60 to 80 times more than general population) [1,2].
The time interval between the diagnosis of Hashimoto's thyroiditis and the development of malignant lymphoma is approximately 9 to 10 years [2].
Due to the underlying risk factors, primary thyroid lymphomas occur more often in women than men (8:1), not the case in our small series, and usually around 6th -7th decade [3].
Patients often present a rapidly enlarging goiter associated with other symptoms including dyspnea, dysphagia, and loss of weight or appetite. In some of our cases, the patients presented a large cervical mass with an upper mediastinal invasion resulting in a compression of the vena cava in two patients and a Claude Bernard Horner syndrome in one case [3].
Ultrasound is usually the first imaging modality performed when evaluating a goiter, three categories of findings were the most described; diffuse glandular heterogeneity, nodular lesions, or the association of both [4].
Fine needle aspiration cytology and/or biopsy are very important in such cases, confirming the diagnosis before the surgery, an often unneeded procedure (unless complications) [4,5].
The choice of adequate treatment is based in the histological subtype; the stage, the tumor bulk, as well as other associated co-morbid factors. As mentioned, the most frequently encountered histological type is B-cell origin and predominantly of diffuse large-cell type, the second most common type is MALT lymphoma, other less frequent types are Hodgkin's disease, Burkitt's lymphoma, plastocytoma and T-cell lymphoma [6].
The staging is adopted from the Ann Arbor system. Its work up involves physical examination, blood tests including beta-microglobulin and lactate dehydrogenases, radiological imaging including CT, MRI Nuclear medicine and PET-CT [4,6].
CT and MRI are suitable for defining the local extension of the disease, lymph node involvement. Nuclear imaging is more useful for evaluating the extent of lymph node involvement and distant metastasis [4,6].
Because lymphomas are sensitive to chemotherapy and radiotherapy, the general consensus is to avoid extensive surgery. Most centers preconize the CHOP/R-CHOP chemotherapy regimen (cyclophosphamide, doxorubicin, vincristine and prednisolone) with or without radiation therapy. Litterature cases report often a dramatic reduction in tumor size after this protocol, with remission to IE and IIE grade cases. The 5-year reported survival rate is about 80% for stage IE, 50% for stage IIE and less than 36% for stages IIIE and IVE [5,6].
The diagnosis of primary thyroid lymphoma should be kept in mind when dealing with rapidly growing goiters. Fine needle aspiration cytology and open biopsy helped reduce surgical debulking, which is replaced with radiation therapy and chemotherapy that show good results especially when caught in the early stages.
The authors declare no competing interest.
All the authors contributed to the diagnosis, the work and the write up of the article. All authors have read and agreed to the final version of this manuscript and have equally contributed to its content and to the management of the case.