Septic thrombosis of the lateral sinus is a rare complication of otitis media; currently, it hasn't been found a case report of septic thrombosis of the lateral sinus in the medical literature of Colombia and, in addition to this, there is no consensus in the management of this pathology. Hence the importance of the present case, which is a 3-year-old male patient, who presented a clinical picture of 7 days of evolution characterized by right otalgia and fever, which after the administration of amoxicillin for 5 days got complicated and showed symptoms of severe headache, photophobia, nausea and vomiting. An extra-institutional computed tomography was performed, where thrombosis of the right lateral sinus and bilateral mastoiditis was evidenced, therefore it was remitted to the Misericordia Hospital in Bogotá, Colombia, where the treatment with intravenous ceftriaxone started, it was requested a magnetic resonance that confirmed the diagnosis and it was decided to perform right mastoidectomy and tympanostomy with ventilation tubes insertion, after this the patient was treated with low molecular weight heparin for 3 months and, in the long term, he presented a favorable evolution.
Lateral sinus thrombosis, Otitis media, Case reports, Pediatrics
Acute otitis media (AOM) is a common disease in children populations, from 50% to 90% of the children from 0 to 5 years have suffered at least one episode of otitis media, peaking between the 6 to 12 months. Most of the time is a benign episode [1].
Septic lateral sinus thrombosis (LST) is an intracranial complication of acute/chronic suppurative otitis media, which is between 2% to 20% of the intracranial complications. Septic LST is the formation of thrombi in the sigmoid/transverse sinus and it can reach the jugular bulb and the internal jugular vein. LST has decreased since the introduction of treatments with antibiotics for media otitis, its mortality rate ranges from 5% to 10% [2,3] and it has morbidity of 30%.
There are two pathophysiological mechanisms of the LST: One happens when acute otitis produces erosion of the bone that protects the sigmoid sinus and it causes an inflammation of the walls, which influences the formation of thrombi; the other one is the thrombosis that occurs as a result of the thromboembolic extension through the small veins. The diffusion of the infection from the inner ear to the sigmoid sinus occurs between the mastoid bridging veins and the intraosseous vessels through the haversian canals [3-5].
The clinical presentation is variable; the most common symptoms are headache, otalgia, vomiting, giddiness, visual disturbance and neck pain, while the most common signs are fever, swelling, ear discharge and mastoid swelling [2].
Predisposing factors of LST have been noted, such as: secondary antibiotics resistance in patients with frequent otitis media, suppurative otitis media and thrombophilia. Because of the last named factor, it is necessary to request coagulation tests [6].
A computed tomography without contrast (CT scan) can be performed in order to confirm the diagnosis of lateral sinus thrombosis. The Nuclear magnetic resonance (NMR) angiography is the most accurate technique, because it shows the vessels and the presence of thrombosis in them, an endoluminal subtraction corresponding to the thrombus and it also helps to specify the size of the thrombus and check the integrity of the contralateral sigmoid sinus [1,5,7].
This complication is treated with antibiotic therapy targeting anaerobic and aerobic microorganisms, surgery (mastoidectomy) and, in some cases, anticoagulant.
Currently, it hasn't been found a case report of septic thrombosis of the lateral sinus in the medical literature of Colombia and, in addition to this; there is no consensus in the management of this pathology, hence the importance of the present case.
3-year-old male patient, who showed a clinical picture of 7 days of evolution with symptoms of right sided otalgia and fever. He was diagnosed with right sided acute otitis media, first episode, with no risk factors nor significant background and he received oral antibiotic treatment (amoxicillin 90 mg/kg per day), after 5 days of the treatment he showed persistent frontal headache, photophobia, nausea and vomiting, therefore an extra-institutional brain CT scan was requested, which showed suggestive signs of thrombosis in the right lateral sinus and bilateral mastoiditis (Figure 1 contrast CT brain shows "delta" sign on lateral sinus and right sided sigmoid). The patient was referred to the Misericordia Hospital in Bogotá, Colombia, where the treatment with intravenous ceftriaxone started.
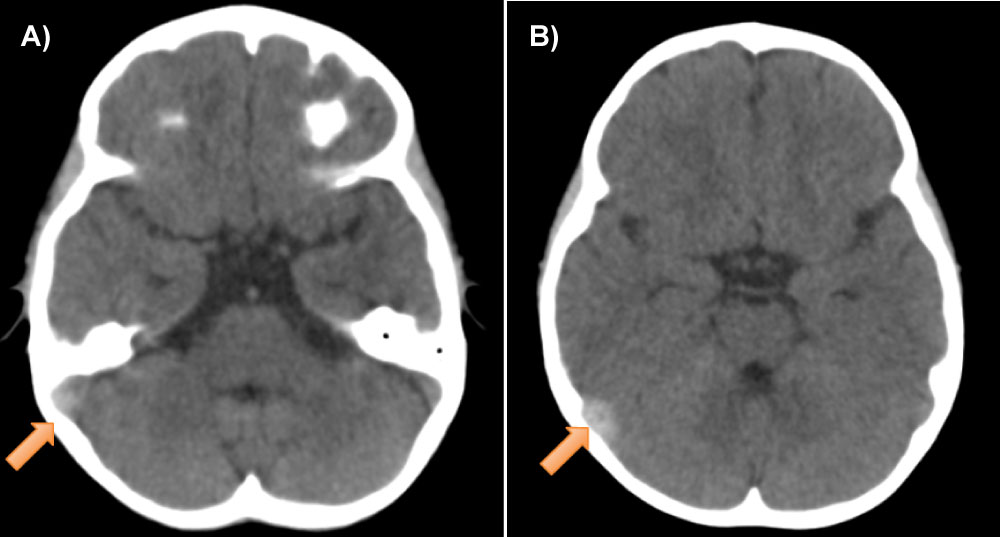 Figure 1: Contrast CT brain shows "delta" sign on lateral sinus and right sided sigmoid. View Figure 1
Figure 1: Contrast CT brain shows "delta" sign on lateral sinus and right sided sigmoid. View Figure 1
Afterwards the patient was evaluated by pediatric neurology, who requested a magnetic resonance angiography. The results confirmed the diagnosis and it was requested an evaluation by otolaryngology.
At the time of the evaluation made by otolaryngology the patient was afebrile, hemodynamically stable, without nuchal rigidity and without neurological symptoms. During the otoscopy, the tympanic membrane was found bulging and opaque, it showed a negative pressure during the pneumatoscopy and it was performed a contrast CT brain, where appeared the "delta" sign on the lateral sinus and the right sided sigmoid (Figure 1). In the inner ear CT (Figure 2) was shown density of the soft tissues, mastoid cells and tympanic cavity without erosion of the sigmoid nor cortical sinus and there was no injury of the otic capsule.
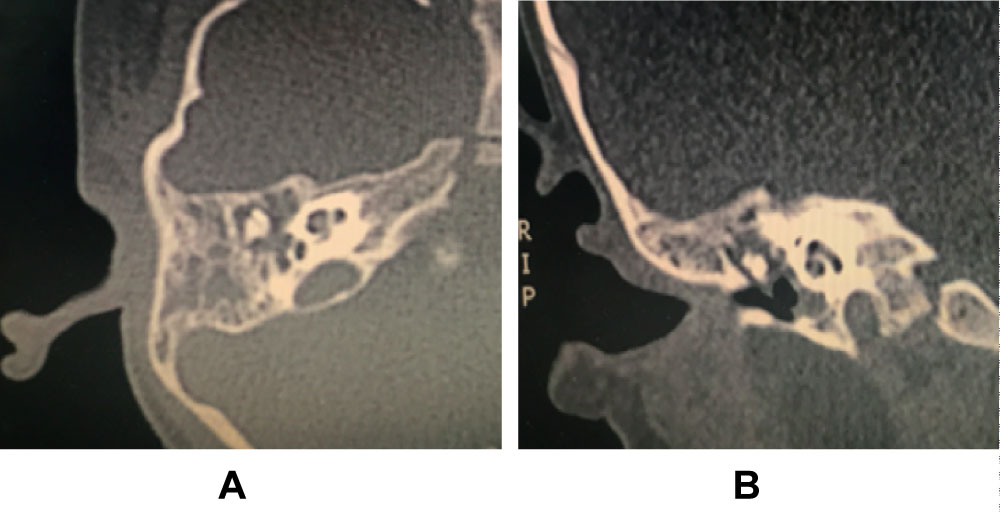 Figure 2: Inner ear CT scan shows density of the soft tissues, mastoid cells and tympanic cavity. View Figure 2
Figure 2: Inner ear CT scan shows density of the soft tissues, mastoid cells and tympanic cavity. View Figure 2
Among the tests performed on the patient, C-reactive protein (CRP) was found in normal ranges, normal blood count without leukocytosis and a laboratory work-up for thrombophilia was performed that included complete blood count, protein C, protein S, antithrombin III, factors VIII, IX, and XI, which were all in normal ranges. During the audiometry, the PTA was of bilateral 15 DB; in the brain magnetic resonance arthrography (Figure 3) was shown thrombosis of the lateral sinus and right sided sigmoid, therefore it was decided to perform right mastoidectomy and tympanostomy with ventilation tubes insertion, a right retroauricular approach was performed, with mastoid decortication and mastoidectomy wall up to the limits, then the tympanostomy was performed with the placement of the ventilation tubes, among the intraoperative findings the presence of serohematic secretion in the transtympanic puncture and abundant inflammatory mucosa in the mastoid vertex are highlighted, samples were taken for culture, which were negative, the procedure worked well, after this the patient was treated with low molecular weight heparin, dalteparin, for 3 months. The patient progressed well and showed a favorable prognosis.
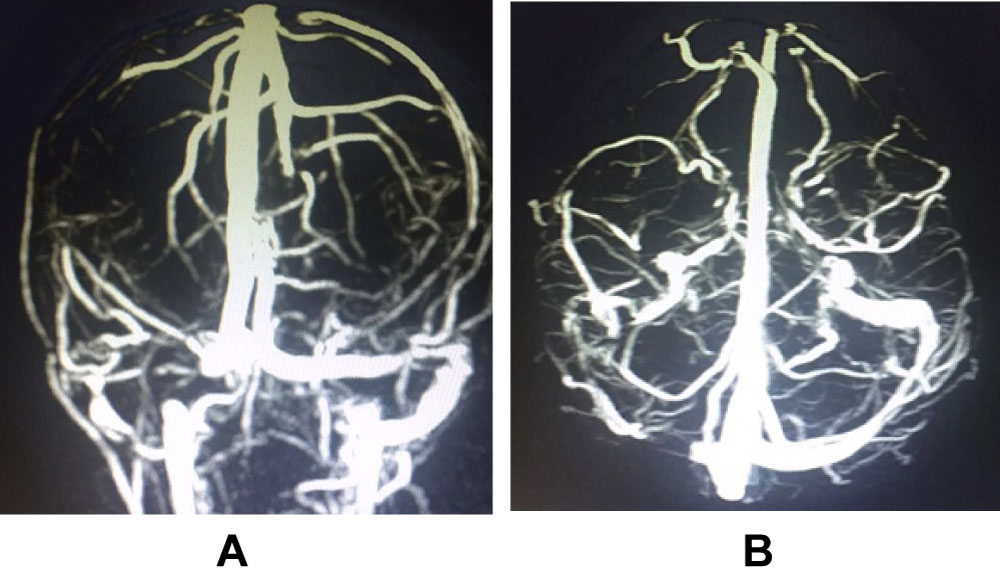 Figure 3: Arthrography through nuclear magnetic resonance of brain, 3D reconstruction, shows filling defect in lateral sinus and right sided sigmoid. View Figure 3
Figure 3: Arthrography through nuclear magnetic resonance of brain, 3D reconstruction, shows filling defect in lateral sinus and right sided sigmoid. View Figure 3
In the present case the patient showed otalgia, fever, headache, nausea and vomiting, which is consistent with a patient cohort, where most common signs and symptoms found were fever (88%), otalgia (77%) and ear discharge (55%), followed by neurological findings such as headache, abducens nerve palsy and papilledema (44%) [2].
When there is a suspicion of LST the final diagnosis is taken through the realization of a contrast-enhanced magnetic resonance venography with a 3D reconstruction, since it has a 90% of sensitivity and a 96% of specificity [8].
According to the review of the literature carried out, LST is treated with antibiotics against aerobic and anaerobic organisms with duration of 4 to 6 weeks. It was also found that an early surgery it is essential [9].
The surgical management is based on simple mastoidectomy or modified radical mastoidectomy, with the removal of the surrounding granulation tissue, the surgical management must be personalized in each patient. A modified radical mastoidectomy is realized when the patient has cholesteatoma, otherwise a simple mastoidectomy it's done. In some cases found during the literature review, it was realized an incision of the lateral sinus for the eventual removal of the clot; however, there are some studies showing that the prognosis doesn't improve by the exploration of the sinus nor the removal of the clot [2]. In another cases the procedure is done with mastoidectomy along with the insertion of tympanostomy tubes [10], which was also the management realized in this case and it had a favorable outcome.
The presentation age is variable and there is not prevalence of gender or race. It is found a link between the LST, the history of recurrent otitis media and the presence of bleeding disorders, but in the present reported case the patient hadn't these medical histories.
In a research carried out in 25 children with lateral sinus thrombosis, it was found that 24 patients (95%) had at least one inherited blood abnormality associated with thrombophilia; the most common finding was the methylenetetrahydrofolate reductase (MTHFR) C677T mutation, it was found in 20, 80% of the cases. This finding was followed by the protein S deficiency found in 11, 44% of the cases and the factor V Leiden mutation presented in 6, 24% of the patients [9]. In another research, where 7 patients with LST participated, it was found blood disorders in 3 patients, reduction of the level of serum proteins C and S, high levels of factor IX and high levels of anticardiolipin antibodies [10].
Because of the relation between thrombophilia and pediatric LST as a secondary complication to media otitis, it is concluded that LST can exhibit a hidden thrombophilia, therefore it's necessary the realization of a laboratory study to rule out thrombophilia and it's also necessary the anticoagulant treatment in the management of patients with both complications [10].
However, according to medical literature, there is no consensus about the use of anticoagulation. Reviewing the world medical literature, it can be observed that in 8 of 16 case reports or case series was used the anticoagulation during the treatment and there were no side effect reported associated to this management. In the present case report, it was also performed the anticoagulant treatment and there were no adverse events, it is observed that the majority of the cases, in which anticoagulants where used, were pediatric patients. When anticoagulant management wasn't performed, the studies were carried out on adults.
In some reports, where coagulation wasn't used, it is stated that anticoagulants must be used only when the thrombus spreads proximally to the internal jugular vein or grows in a retrograde direction to the most distal intracranial sinuses, since there is risk of venous infarcts with their use [4]. It has also been proved that the venous sinus recanalization occurs without anticoagulation after the surgical extraction of the mastoid and epidural infection and after the 6 weeks treatment with antibiotics [3].
It is recommended to use in newborns, initially, anticoagulant treatment with unfractionated heparin (28 u/kg/h) or low molecular weight heparin (1.5 mg/kg every 12 hours and intravenous), followed by low molecular weight heparin or warfarin for 6 to 12 weeks. Older children should receive initially unfractionated heparin (20 u/kg/h) or low molecular weight heparin (1 mg/kg every 12 hours and intravenous), followed by low molecular weight heparin or warfarin for 6 months [10].
The anticoagulant treatment in the cases reviewed went on for 3 months on average and with favorable outcomes. Some of the benefits found of the use of the anticoagulant treatment are: It limits the propagation of the thrombus, it increases the intracranial venous drainage and it reduces the effects of an increased intracranial pressure, meaning an improvement of the neurological state [3].
It is also questioned if the ligation of the internal jugular vein helps, however it has been found that this surgery is indicated if blood clots extend beyond the mastoid area, if sepsis and pulmonary complications persist despite the initial treatment with surgery and if an infection or thrombosis of the internal jugular vein is found [4].
It is concluded that although LST as a complication of AOM in children is a rare complication, there must be suspicion in order to make a timely diagnosis and avoid complications. In the present case report was used antibiotics, it was performed mastoidectomy and tympanostomy with ventilation tubes and anticoagulant treatment, as currently appears in medical literature, which gave the patient a full recovery. Researches statistically more significant are needed to specify the indications and contraindications of the anticoagulant treatment.
The consent of the patient of the reported case was received and there is no conflict of interest.