Otitis media with effusion (OME) is an important and common condition in paediatric age group. It is the leading cause of hearing loss and a social morbidity in children which has long-term consequences for speech and language development [1]. Adenoid hypertrophy is an important etiological factor in the causation of OME. Recurrent attacks of rhinitis, sinusitis and chronic tonsillitis may cause chronic adenoid infection and hyperplasia. Allergy of the upper respiratory tract may also contribute to enlarged adenoids [2]. The main reasons postulated for adenotonsillectomy as a means of treatment and prevention of recurrence have centred on the size of the adenoids and the role of recurrent tonsillitis as a focus for ascending eustachian tube infection.
Symptoms due to adenoid and tonsillar hypertrophy include nasal obstruction, snoring, mouth breathing and hyponasal speech. Enlarged adenoids block the eustachian tube causing conductive hearing loss. The classical concept is that enlarged adenoid or recurrent infection of adenoids causes recurrent acute otitis media and OME. The normal middle ear pressure is -100 mm of H2O to + 50 mm of H2O and the normal middle ear compliance is 0.39 ml to 1.30 ml. Enlarged adenoid causes tubal obstruction at its nasopharyngeal opening and causes reduction of middle ear pressure and compliance towards negative side due to absorption of gas which leads to otitis media with effusion [3]. Local symptoms and signs include hearing loss, feeling of fullness in the ear, a 'popping' sensation and a dull retracted tympanic membrane (TM) with restricted mobility on saegalisation often with air bubbles behind the TM. Increased pressure can also cause a bulging TM.
Tympanometry is a noninvasive test used for measuring middle ear pressure. OME commonly presents with a type B curve i.e, a flat curve with no compliance peak. Other abnormal tympanometric curves including type C and As may also be seen in OME. Pure tone audiometry (PTA) has been the gold standard for the evaluation of hearing level [4]. A comparison of thresholds measured by air conduction (AC) and bone conduction (BC) provides separate estimates of the status of conductive and sensorineural systems. However, PTA being a subjective test fails to provide adequate assessment in very young children.
Auditory steady-state response (ASSR), a newly developed objective auditory evoked potential test predicts frequency specific hearing threshold in all patients irrespective of age, mental state, and the degree of hearing loss. ASSR being an objective test, can be easily used in infants and children while they are sedated or asleep to assess the degree of hearing loss [5]. Post adenotonsillectomy there is an improvement in Eustachian tube function and reduction in middle ear effusion. The gain in hearing can be quantified by a post operative ASSR. On searching the english literature, we couldn't find any published study assessing the changes in ASSR post adenotonsillectomy in OME. Therefore, this prospective study was planned with a specific objective to evaluate the effect of adenotonsillectomy in treatment of recurrent secretory otitis media in children and the evaluation of its effect on hearing with ASSR.
With the approval of the ethical committee of our institute, a prospective study was conducted on randomly selected 20 patients (40 ears), with recurrent otitid media with effusion (OME), of either sex attending the ENT out patient department of Post Graduate Institute of Medical Sciences, Rohtak, India. Patients in age group of 5-15 years with bilateral conductive hearing loss of more than 25 db, having adenotonsillar hypertrophy confirmed by clinical examination and x-ray soft tissue nasopharynx. All these patients underwent adenotonsillectomy after unsatisfactory medical treatment. The patients having a perforated tympanic membrane, cleft palate and other congenital anomalies of ear, recurrent rhinosinusitis and allergic rhinits were excluded from the study.
The size of adenoids was assessed with the help of x-ray soft tissue skull lateral view and graded as follows [6].
Grade I-adenoid occupying less than 25% of nasopharynx.
Grade II-adenoid occupying 25% to 50% of nasopharynx.
Grade III-adenoid occupying 50% to 75% of nasopharynx.
Grade IV-adenoid occupying 75% to 100% of nasopharynx.
Tonsillar hypertrophy was graded by Friedman's Grading [7]. In grade-I hypertrophy, the tonsils were hidden in the tonsillar fossa and were barely visible behind the anterior pillars. In grade-II, the tonsils were visible behind the anterior pillars and occupied up to 50% of the pharyngeal space (the distance between the medial borders of the anterior pillars). In grade-III, the tonsils occupied between 50 and 75% of the pharyngeal space. In grade-IV, the tonsils occupied more than 75% of the pharyngeal space.
After an informed written consent, patients underwent adenotonsillectomy under general anaesthesia. Adenoidectomy was carried out using St. Clair Thompsons adenoid currete and tonsillectomy was done by dissection method under general anaesthesia. Oral hygiene was maintained with help of betadine and hydroxyl gargles. Infusion paracetamol was given as anaelgesia. The pure tone audiometry (PTA), ASSR and impedence audiometry were performed in all the patients preoperatively and 8 weeks after adenotonsillectomy on achieving complete healing. Our study was a case control study/repeated measures design. The paired-t test was applied on the recorded data. All tests were performed at 5% level of significance, thus an association was significant if the p value was less than 0.05.
• In this study, patients ranged between 5-15 years of age with mean age of 6.70 ± 2.598 years. There were 12 males (60%) and 8 females (40%). Incidence of male patients is more due to more incidence of childhood infection in males.
• Mouth breathing was the most common symptom (Figure 1).
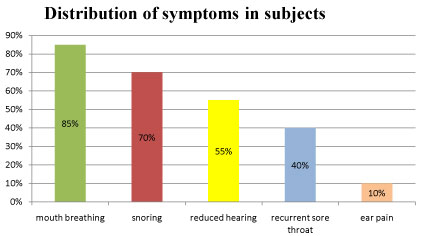 Figure 1: Distribution of symptoms in subjects. View Figure 1
Figure 1: Distribution of symptoms in subjects. View Figure 1
• Adenoid facies were present in 14 patients, accouting for 70% of patients.
• According to radiological grading, six patients were having grade II adenoids (30%), 6 were having grade III adenoid hypertrophy and 8 (40%) were having grade IV adenoid hypertrophy. Mean adenoid hypertrophy grade of subjects was 3.10 ± 0.85224.
• Out of 20 patients, 11 were having grade III tonsillar hypertrophy (55%), 7 were having grade II tonsillar hypertrophy (35%) and 2 were having grade IV tonsillar hypertrophy. Mean tonsillar hypertrophy was 2.75 ± 0.639.
• On preoperative otoscopy, majority of patients had either a bulging or a retracted tympanic membrane and only 10% tympanic membrane were normal in appearance. On post operative otoscopy, 33 (82.5%) tympanic membranes were normal (Figure 2 and Figure 3).
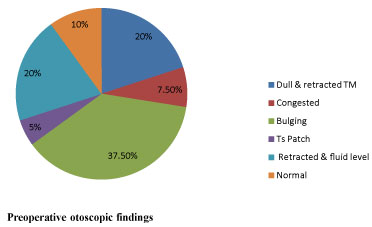 Figure 2: Preoperative otoscopic findings. View Figure 2
Figure 2: Preoperative otoscopic findings. View Figure 2
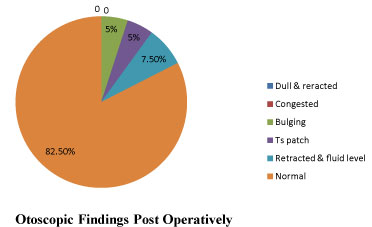 Figure 3: Otoscopic findings post operatively. View Figure 3
Figure 3: Otoscopic findings post operatively. View Figure 3
• Only 15 out of 20 patients gave reliable response on PTA (n = 30 ears). The mean preoperative Air Borne (AB) Gap (dB) on PTA was 25.23 ± 10.67 dB while the mean postoperative AB Gap (dB) was 14.27 ± 7.61 dB. The mean gain in AB Gap (dB) is 10.97 ± 12.18. P value was 0.000031 which is less than 0.05, making the hearing improvement significant.
• The mean preoperative hearing loss on PTA (AC) was 43.23 ± 12.13 dB while the mean postoperative hearing loss on PTA (AC) is 27.66 ± 7.967 dB. The obtained p value was 0.00969 which is less than 0.05 making hearing improvement statistically significant (Table 1).
Table 1: Comparison of Preoperative and Postoperative PTA (n = 30). View Table 1
• ASSR could be conducted in all patients (n = 40 ears). The mean preoperative ASSR (dB) was 41.56 ± 11.05 dB while the mean postoperative ASSR (dB) is 24.65 ± 8.47 dB. The mean gain in hearing (dB) is 16.95 ± 11.89 and p value is less than 0.05 showing significant improvement in hearing (Table 2) (Figure 4).
 Figure 4: Comparison of Pre and Postoperative ASSR. View Figure 4
Figure 4: Comparison of Pre and Postoperative ASSR. View Figure 4
Table 2: Comparison of Preoperative and Postoperative ASSR (n = 40). View Table 2
• Maximum ears were having B type of curve (62.5%) followed by C type of curve (30%) preoperatively. Maximum cases were of type A curve (70%) postoperatively. B and C type curves were considered reflective of OME (Table 3).
Table 3: Preoperative and Post opertaive tympanogram in 40 ears (n = 40). View Table 3
• On comparing adenoid hypertrophy with middle ear pressure assessed by impedance audiometry we found that with grade II adenoid hypertrophy, there were 8 ears with >+ 150 dPa pressure, 3 with -150 dPa pressure and 1 with pressure between -150 to +150 dPa. With grade III adenoid hypertrophy, there were 6 ears with >+ 150 dPa, 4 with pressure between -150 to +150 dPa and 2 with -150 dPa pressure (Table 4), (Figure 5).
 Figure 5: Preoperative middle ear pressure with Adenoid hypertrophy grade (x-axis). View Figure 5
Figure 5: Preoperative middle ear pressure with Adenoid hypertrophy grade (x-axis). View Figure 5
Table 4: Statistical analysis of preoperative and postoperative middle ear pressure. dddView Table 4
In our study, the mean age of subjects was 6.70 ± 2.598 years (range 5-15 years). In a study by Maw, children ranging from 2-11 years with a mean age of 5.25 were included [8]. In present study majority of children belonged to the age group 5-6 years (65%) which was followed by the 7-9 year group (20%). This observation is in concurrence with a study of Fujioka, et al. which showed that the size of the adenoid, though varies from child to child, the adenoids attain their maximum size between 4-8 years of age after which it regresses gradually till the age of 15 years [9]. In the present study out of 20 patients, there were 12 males (60%) and 8 females (40%). This could be attributed to more incidence of infection in male children and an increased concern for male children by parents in this state.
In present study 17 (85%) had complaints of mouth breathing, snoring was present in 14 patients (70%) and reduced hearing was present in 11 patients (55%). The predomination of nasal symptoms over aural symptoms may be because identification of nasal symptoms more easily by parents as compared to aural symptoms secondary to adenoids. In this study, adenoid facies were seen in 70% of children. Adenoid facies were seen in 91.4% of children in study by Ajayan, et al. [10].
The current study showed varied appearance of tympanic membrane in the children. A retracted tympanic membrane with or without air fluid level was seen in 40% and 37.5% were having a bulging tympanic membrane. All the above patients showed absent tympanic membrane movements on pneumatic otoscopy, which is a reliable sign of OME. In a study by Satish, 64% ears had a retracted membrane and 16% had air bubbles and 94% had a dull, amber coloured membrane [11].
In this study in preoperative impedence audiometry, 'B' type of curve was present in 25 ears (62.5%), 'A' type of curve found in 1 ear (2.5%), 'C' type of curve was found in 12 ears (30%) & 'As' curve was seen in 2 ears (5%). In study by Abd Alhady et al. among 40 cases (2-6 years old) with adenoid enlargement, 23 cases showed abnormal tympanometry including five ears with type 'B' and 27 ears type 'C' [12]. Postoperatively maximum patients (70%) had 'A' type of curve in the current study and 17.5% had 'C' type curve.
In the present study complete resolution of OME (suggested by type A tympanogram) was seen in 67.5% of ears 2 months postoperatively. Similar results were seen in the study by Maw, where rate of resolution was 59% at 6 weeks and 62% at one year which he compared with no surgery group [6]. It has been shown in many studies that the hearing loss in OME shows a wide range with air conduction thresholds averaging 27.5 dB [13]. In the current study the mean preoperative ASSR (dB) was 41.56 ± 11.05 dB. Since ASSR is an objective test, it was advantageous over PTA as all patients could be assessed. However, when PTA was carried out only 15 patients responded properly to the changes in amplitude. The mean preoperative hearing threshold in PTA (dB) being 42.93 ± 12.42 dB (range 20-70 dB) which almost correlates with a study by Dong and Wang where the average air conduction ASSR threshold in patients with OME at 0.25 kHz was 42 ± 15 dB [14].
In our study, the mean gain in hearing (dB) in ASSR of all ears(n = 40) was 16.95 ± 11.89. The p value is less than 0.05, making it statistically significant. This was comparable with the gain in hearing in PTA which was 15.27 dB (n = 30). Similar gain of 14.25 dB in PTA was seen at 3 months post surgery in the study by Ajayan, et al. [10]. According to Black, et al. the mean dB gain at 7 weeks and 6 months were 4.5 and 3.5 dB respectively [15].
When the hearing loss was compared with the size of adenoid, it was seen that there was no significant correlation between the grade of adenoid hypertrophy and the degree of hearing loss. There was no significant correlation between the size of adenoids and middle ear pressure in our study. On comparing adenoid hypertrophy with middle ear pressure assessed by impedance audiometry in our study, the p value is 0.658 which is statistically non significant, yet higher values of middle ear pressure are associated with higher grades of adenoid hypertrophy. Similar results were obtained by Khayat, et al. as they observed that the incidence of abnormal tympanometry was higher with an increased adenoid size but it was statistically non-significant [16]. However, in a study by Zaman and Borah they concluded that the size of the adenoids had a nearly significant effect on the pre-operative middle ear pressure [17]. Abdul Latif, et al. showed that removal of adenoid results in resolution of OME [18]. However, recurrent or chronic infection in adenoid without eustachian tube lumen obstruction may cause acute otitis media and OME supporting the fact that adenoid can be a reservoir for pathogens that can lead to Eustachian tube oedema and dysfunction. Takahashi, et al. mentioned that adenoidectomy benefits relate to removal of infection source rather than mechanical obstruction and found same infection pathogens in the nasopharynx of children with OME [19]. Many other studies have been carried out which compare adenoidectomy in OME with insertion of tympanostomy tubes with or without adenoidectomy. They also concluded that the children in the adenoidectomy groups experienced significantly less time with effusion and fewer repeat surgeries [20-22].
Our study shows a significant benefit of adenotonsillectomy as far as the resolution of middle ear effusion in children with otitis media with effusion (OME) with adenotonsillar hypertrophy which were not controlled by medical treatment alone, is concerned. The improvement in hearing is also significantly noted on both ASSR and PTA, alongwith the resolution of changes in the tympanic membrane in these patients. However, the risks of operation should be weighed against these potential benefits. Also, ASSR can be reliably used for determining the hearing threshold especially in very young children who are not cooperative with PTA.
None.