A 66-year-old male experienced right sided shin and calf pain of an insidious onset. The duration of pain was 3 months, aggravated by walking and running. He also reported resting pain especially during the night. A detail medical evaluation ruled out the presence of a blood clot and electrolyte imbalance. He was diagnosed as having restless leg syndrome and referred for physical rehabilitation. Initial examination revealed positive findings of comparable local tenderness over the right shin and calf. He also presented with foot pronation that persisted throughout the stance phase of gait. Hence his ability to reverse pronation was tested in the standing position. With the knees completely extended, he presented with an inability to actively supinate and dorsiflex the foot on the right side. 8 treatment visits for a period of 4 weeks addressed mechanical dysfunction at the ankle, foot, and hip region, comprising, manual therapy, corrective exercise and pain modalities. Reduction of local tenderness, and activity related shin and calf pain was observed. He reported continued discomfort at rest, but of a minimal intensity. Additionally, full range of active supination and dorsiflexion was restored in the standing position with the knees completely extended. The findings in this case report describe a common cause of shin pain. It highlights a novel and easily administered method of evaluating limited mobility in the talocrural joint and the relative inability to supinate the foot that could potentially contribute to the symptomatology. The test was of value in assessing the need as well as the outcome of rehabilitation intervention. Further research to examine the diagnostic utility of this method is recommended.
Leg pain, Pronation, Reversal, Supination, ASDT
Lower leg, shin and calf pain are frequently encountered in rehabilitation settings. It is a condition prevalent in both active and sedentary individuals [1,2]. Individuals presenting to a primary care setting with lower leg, shin and calf pain are evaluated for the possible presence of blood clots [3], chronic exertional compartment syndrome (CECS) [4], stress fractures [5], and infrequently malignancy [6]. Other causes for lower leg and shin pain described in the literature are medial tibial stress syndrome (MTSS), popliteal artery entrapment syndrome (PAES) [7-10], peripheral neuropathy, lumbar radiculopathy, spinal stenosis [9,10], dehydration [11], vitamin B12 and vitamin D deficiency [12,13], exertional rhabdomyolysis [14], restless leg syndrome [15], varicosities [16], congestive cardiac failure [17] and renal pathology [18].
The most common etiologies for mechanical lower leg pain are extended periods of running [1,7,8] and prolonged periods of standing and walking [19-21]. Although a wide range of diagnoses exist for mechanical and activity-induced leg pain, MTSS, CECS, stress fracture, nerve entrapment, and PAES are the most common [1]. Often, more than one of these diagnoses co-exist as in MTSS and CECS alongside ankle and foot pain, owing to similarities in their intrinsic and extrinsic risk or aggravating factors [22,23].
The main aggravator described is the altered foot mechanics during the stance phase of gait. Deviations in normal foot and ankle mechanics have been described as causes for mechanical shin, leg, and calf pain [24,25,20]. Literature describes a correlation between lower leg, shin and calf pain and hyper pronation. In a study that prospectively examined the gait-related risk factors for exercise-related lower leg pain (ERLLP) in a young, physically active population, subjects showed significantly increased pronation, accompanied by more pressure underneath the medial side of the foot [20,24,25]. These studies describe pronation as increased ankle plantar flexion from mid-stance to toe-off and less ankle inversion at the end of stance and early swing phases. These two features favor the presence of prolonged pronation and the inability to reverse into supination to offer a rigid lever for push off [26]. Persistent rearfoot plantar flexion during gait increased demand on the anterior compartment musculature during ambulation, resulting in pain and dysfunction [20,27]. For much of the diagnoses of lower leg pain described above, the management and reversal of prolonged pronation of the foot during the stance phase of gait has been advocated, with favorable outcomes [28,29]. The reversal entailed dorsiflexion of the talocrural and inversion of the subtalar joints, to elevate the medial longitudinal arch [27,53,54].
Evaluation methods described in the literature to identify pronation have been both qualitative and quantitative. Navicular drop, subtalar neutral, windlass test, observing for the presence of a flattened medial longitudinal arch and gastrocnemius tightness associated with limited dorsiflexion and are some of them [30-32]. While a single method of assessment may not improve the statistical likelihood of the presence of pronation, a cluster of findings may offer more validity. This case report suggests a novel and easily administered dynamic clinical test that may be added to the cluster, the active supination dorsiflexion test (ASDT). It is proposed that the ASDT may be sensitive to the patho-mechanical challenges that occur during the stance phase of gait in the presence of prolonged pronation or in the absence of reversal of pronation. The test aims to capture the inability of the foot to be able to reverse into supination in preparation for propulsion [27,53,54].
While pronation has been described to cause lower leg symptoms, studies have suggested that muscle imbalance between the invertors and evertors, in the absence of prolonged pronation, also cause similar symptoms [33]. MTSS may occur without pronation indicators like medial longitudinal arch deformation or navicular drop. In such cases, one of the causes described is the strength disbalance of the invertor and evertor muscles in favor of the evertor muscles. It may be of value to know that inversion is a component of supination and a lack thereof can favor dysfunctional pronation [33]. Additionally, the ankle invertor muscles are also dorsiflexors of the ankle and lack of dorsiflexion has also been described as a component of dysfunctional pronation [34,35,38]. Thus, this case report aims to highlight the ability of contractile structures to be able to initiate the windlass mechanism and the reversal of pronation, namely, the foot intrinsics, invertors and dorsiflexors of the foot and ankle [26]. Optimal strength of these muscles is essential for the normal functioning of the foot and ankle.
A 66-year-old retired male who experienced symptoms of right sided shin and calf pain, is presented. The pain was reported to have started gradually over an 8-month period, following bouts of regular 3-5-mile walks and light running. Symptoms began towards the end of his walking sessions and lingered for a few hours. He also reported pain and twitching during the nighttime disturbing sleep. He had worked as a salesman and has been retired for 3 years. He reported his symptoms to his primary care physician. He had a doppler study [36] and an X-ray which revealed negative findings. His blood profile was unremarkable with normal findings in electrolyte values [11]. He was a recovering alcoholic and was on anti-depressants. He presented no other relevant medical history.
Activity especially extended periods of standing and walking typically increased his pain intensity. He reported a relative decrease in symptom intensity with rest and occasionally felt no pain. His pain intensity was 7-8/10 on the Numerical Pain Rating Scale [37] at its worse and 2/10 at best. His primary care physician diagnosed his condition as restless leg syndrome and muscle pain and prescribed pain medication. He was also referred for physical rehabilitation.
The assessment and testing described in this section was done prior to treatment intervention. The patient was seen to be independently ambulant and did not exhibit an antalgic gait. In standing, he presented with a complete loss of his medial longitudinal arch bilaterally. In the standing position, on observation from the posterior aspect he presented with calcaneal eversion. On observation there was no swelling or discoloration of the lower leg with intact dorsalis pedis and posterior tibial pulsation. He reported comparable discomfort and pain over the anterior and lateral shin area and over the mid-calf region. He also reported comparable pain over the medial tibial region. Passive dorsiflexion was limited at 10 degrees on the right side. Active inversion was also terminally restricted on the right side. Plantar flexion and eversion were full and free.
In the standing position the navicular drop test was performed [30]. The distance from the navicular to the ground was measured in a subtalar neutral position and again after the patient was permitted full weight bearing. There was a navicular drop of nearly 2 cm indicating moderate pronation. The windlass test was performed as follows. In the standing position the first metatarsophalangeal joint was extended while allowing the interphalangeal joint to flex. There was no elevation of the medial longitudinal arch with no reproduction of pain in the foot [31]. At this time, the ASDT (Figure 1) was performed with the following operant definition. In the standing position with the knees completely extended, the patient was asked to curl his toes inwards to raise the medial longitudinal arch and invert and dorsiflex the ankle and foot. Knee extension was emphasized to maintain tension of the gastrocnemius which challenged dorsiflexion. He presented with difficulty curling his toes, inverting, and dorsiflexing the foot. Range of motion on active dorsiflexion was 5 degrees on the right and 10 degrees on the left side. Gait assessment revealed the persistence of a flattened medial longitudinal arch throughout stance and into the propulsion phase of gait.
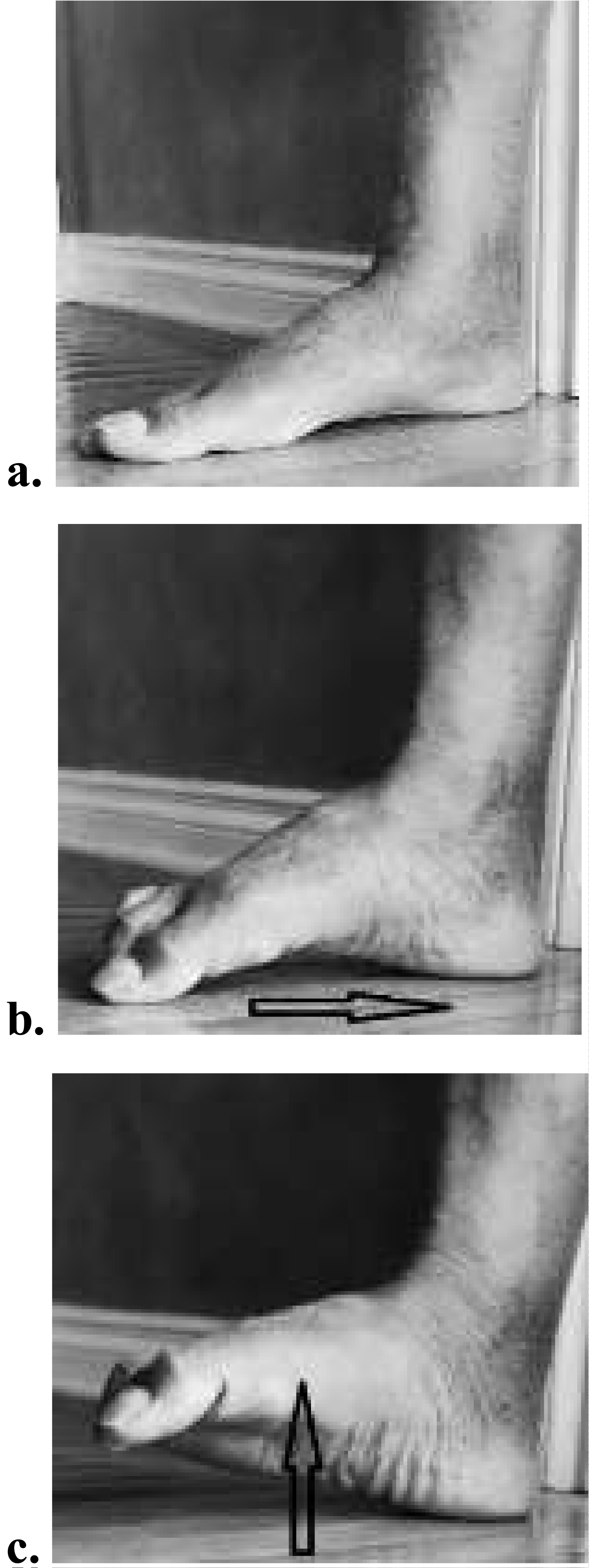 Figure 1: The active supination dorsiflexion test. a) Starting neutral position; b) Intrinsic activation; c) Inversion and dorsiflexion with knee extended.
View Figure 1
Figure 1: The active supination dorsiflexion test. a) Starting neutral position; b) Intrinsic activation; c) Inversion and dorsiflexion with knee extended.
View Figure 1
The overall assessment thus was suggestive of a chronically pronated ankle and foot. In the absence of non-mechanical pathology, the presence of a chronically pronated foot has been shown to correlate to lower leg pain [37]. Additionally, the presence of reproducible anterior and medial shin and calf tenderness made the findings more correlative.
The differential screening process for the current pain presentation recommended ruling out the possibility of a stress fracture, blood clot, compartment syndrome, and electrolyte imbalance. The patient had undergone a detail medical evaluation prior to being referred to physical therapy. This included a visceral screen, blood chemistry analysis, X-rays, and doppler study. He was assured that the findings were negative and suggested that the presentation was musculoskeletal requiring the expertise of a physical therapist.
Given the above findings it was concluded that the patient presented with medial and anterior tibial stress syndrome with mechanical somatic dysfunction of the talocrural and subtalar articulations. The mechanical dysfunction presented as chronic pronation extending into the late and terminal stance phase of gait. This resulted in overuse of the decelerators of pronation namely gastrocnemius, soleus, anterior tibial group of muscles, and the tibialis posterior, causing leg pain and dysfunction [37-40,27].
Based on the clinical findings, the patients age, activity level and general health, it was anticipated that the patient would respond well to treatment and regain normal physiological function and return to pain free participation of his work and leisure activities. The clinical information presented in this case report was in full adherence to the case reporting guidelines set forth by the Henry Ford Health System, Detroit, Michigan.
Treatment addressed mechanical dysfunction at the right ankle and lower leg comprising manual therapy in the form of joint mobilization to the talocrural and subtalar joints (Figure 2 and Figure 3). The intent was to improve dorsiflexion of the talus as a reversal of its plantarflexed position which was favoring pronation [41-43]. This was followed by soft tissue mobilization of the lower leg region addressing the muscles in the anterior and posterior tibial compartments. The intent was to improve blood supply, heating, and plasticity of the tissues, and facilitate synthesis and realignment of new collagen [41]. Exercise prescription began with the patient being instructed in calf stretching to encourage talus dorsiflexion to revert pronation. Care was taken to maintain a neutral supinated position of the foot and ankle to prevent a mid-tarsal over a talocrural stretch [44] (Figure 4). This was followed by open kinetic chain exercises done actively and without resistance. The active exercises targeted the anterior tibial group comprising dorsiflexion and inversion and posterior tibial group comprising plantarflexion and inversion. This was followed by active exercises for the intrinsic foot muscles comprising toe curls over a towel to encourage elevation of the medial longitudinal arch and reversal of pronation (Figure 5). Treatments were concluded with a cold pack over the lower leg region, mainly as an adjunct for its short-term analgesic effect [40].
 Figure 2: Talocrural joint distraction.
View Figure 2
Figure 2: Talocrural joint distraction.
View Figure 2
 Figure 3: Talocrural joint posterior glide.
View Figure 3
Figure 3: Talocrural joint posterior glide.
View Figure 3
 Figure 4: Gastrocnemius stretch.
View Figure 4
Figure 4: Gastrocnemius stretch.
View Figure 4
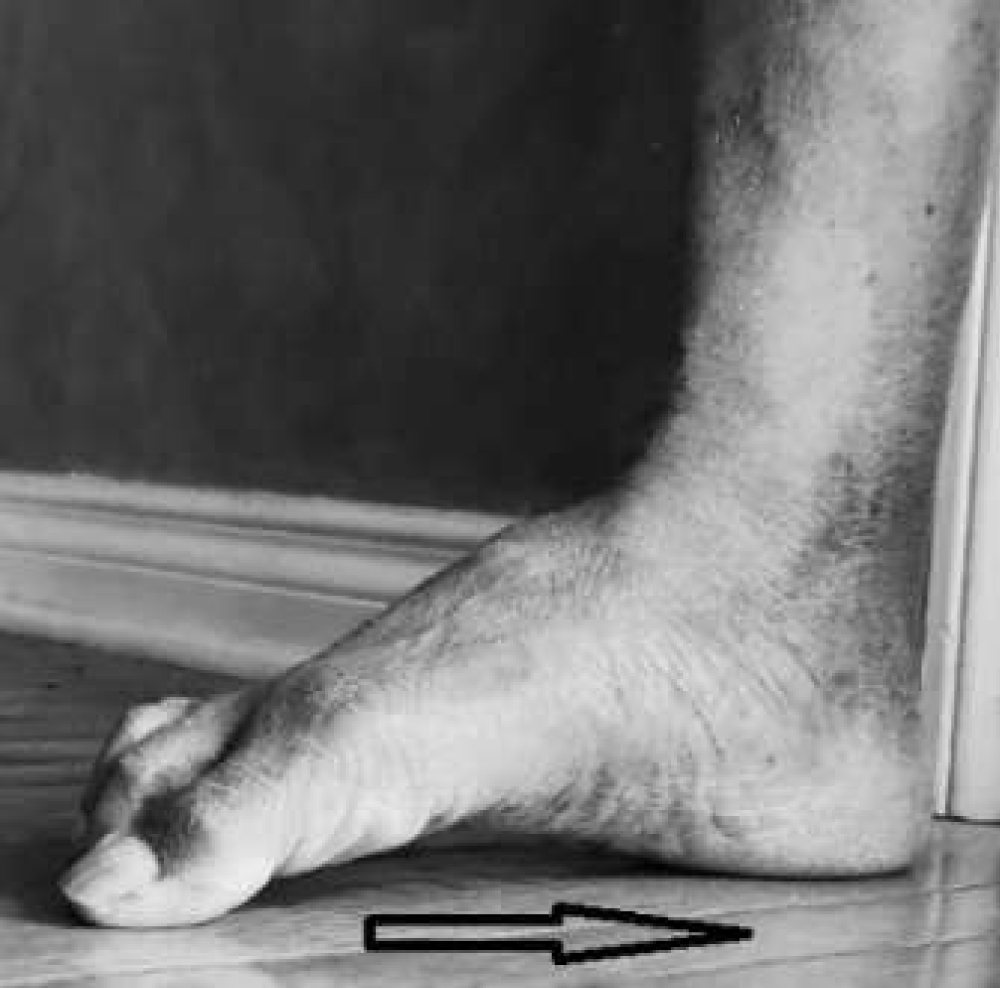 Figure 5: Intrinsic activation without resistance.
View Figure 5
Figure 5: Intrinsic activation without resistance.
View Figure 5
He was wearing a custom-made foot orthotic which controlled pronation by elevating the medial longitudinal arch [46], prescribed by his physician. He mentioned however, that he did not wear it while at home. He was instructed to wear his orthotic during all upright postures, including at home. He was also instructed a home program and was advised to continue his exercises on the days he did not attend therapy sessions. The program was increased in intensity during the third week until the end of the program at 4 weeks. The intensity progression was as follows. Activation of the anterior and posterior tibial group which was initially done without resistance was performed with resistance bands (Figure 6 and Figure 7). Both concentric and eccentric contractions were performed. Ankle and foot strengthening exercises that were done in non-weight bearing were progressed to a weight bearing closed kinetic chain position. Intrinsic muscle activation done over a towel was progressed to adding resistance using a spring-loaded foot exerciser. This was used for progressive strengthening of the intrinsic foot muscles (Figure 8). Additionally, as a progression into weight bearing, he stood over a padded rubber surface and performed the same intrinsic foot exercises with the resistance offered by the padded rubber surface [48,49] (Figure 9). This was done to encourage closed kinetic chain concentric reversal of supination. This was progressed to one legged heel raises with more weight bearing over the lateral border of the forefoot (Figure 10). In the last part of the intensity progression he performed hip abduction and extension in standing with elastic bands of a light resistance, for the gluteus medius and maximus (Figure 11 and Figure 12). This was done to complete activation of the entire lower kinetic chain. Weak gluteal muscles can contribute to dynamic valgus on one legged stance, further contributing to valgus and pronation of the foot [49].
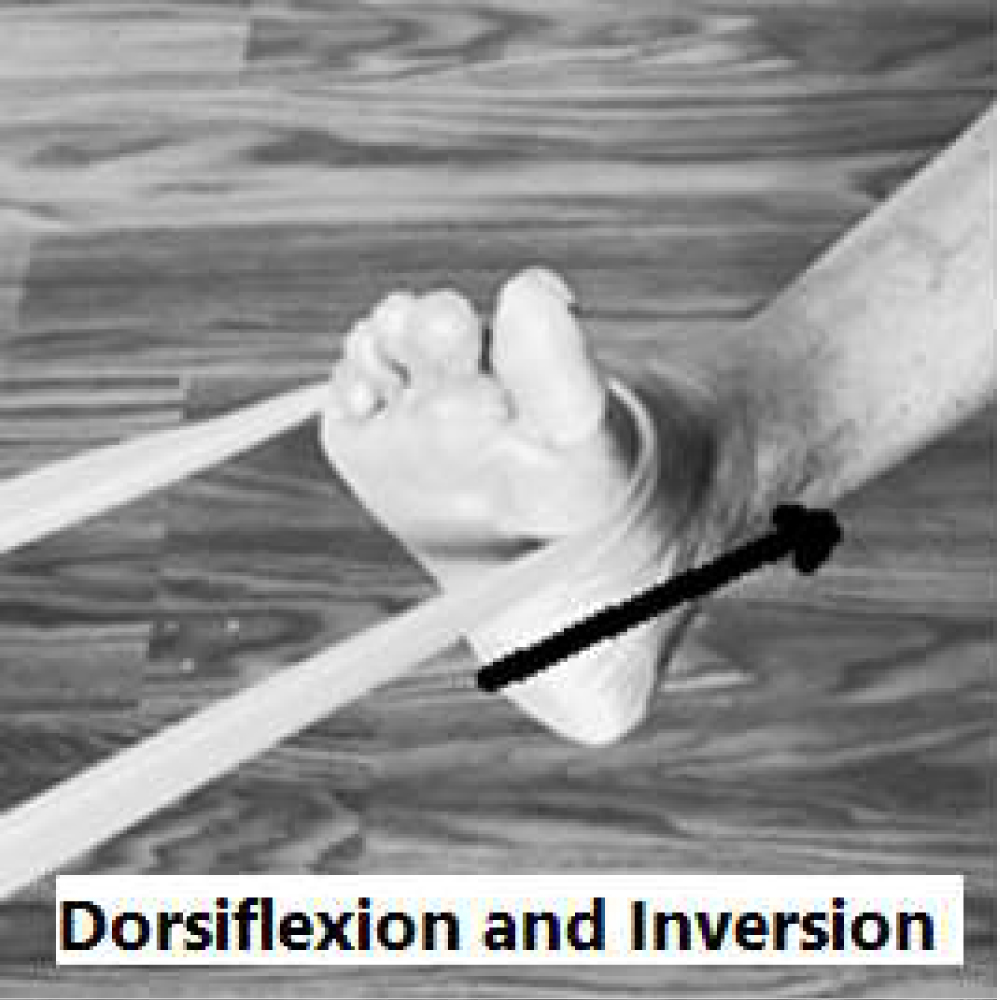 Figure 6: Open chain concentric and eccentric training for tibialis anterior with resistance band and without prior.
View Figure 6
Figure 6: Open chain concentric and eccentric training for tibialis anterior with resistance band and without prior.
View Figure 6
 Figure 7: Open chain concentric and eccentric training for tibialis posterior with resistance band and without prior.
View Figure 7
Figure 7: Open chain concentric and eccentric training for tibialis posterior with resistance band and without prior.
View Figure 7
 Figure 8: Intrinsic activation with resistance.
View Figure 8
Figure 8: Intrinsic activation with resistance.
View Figure 8
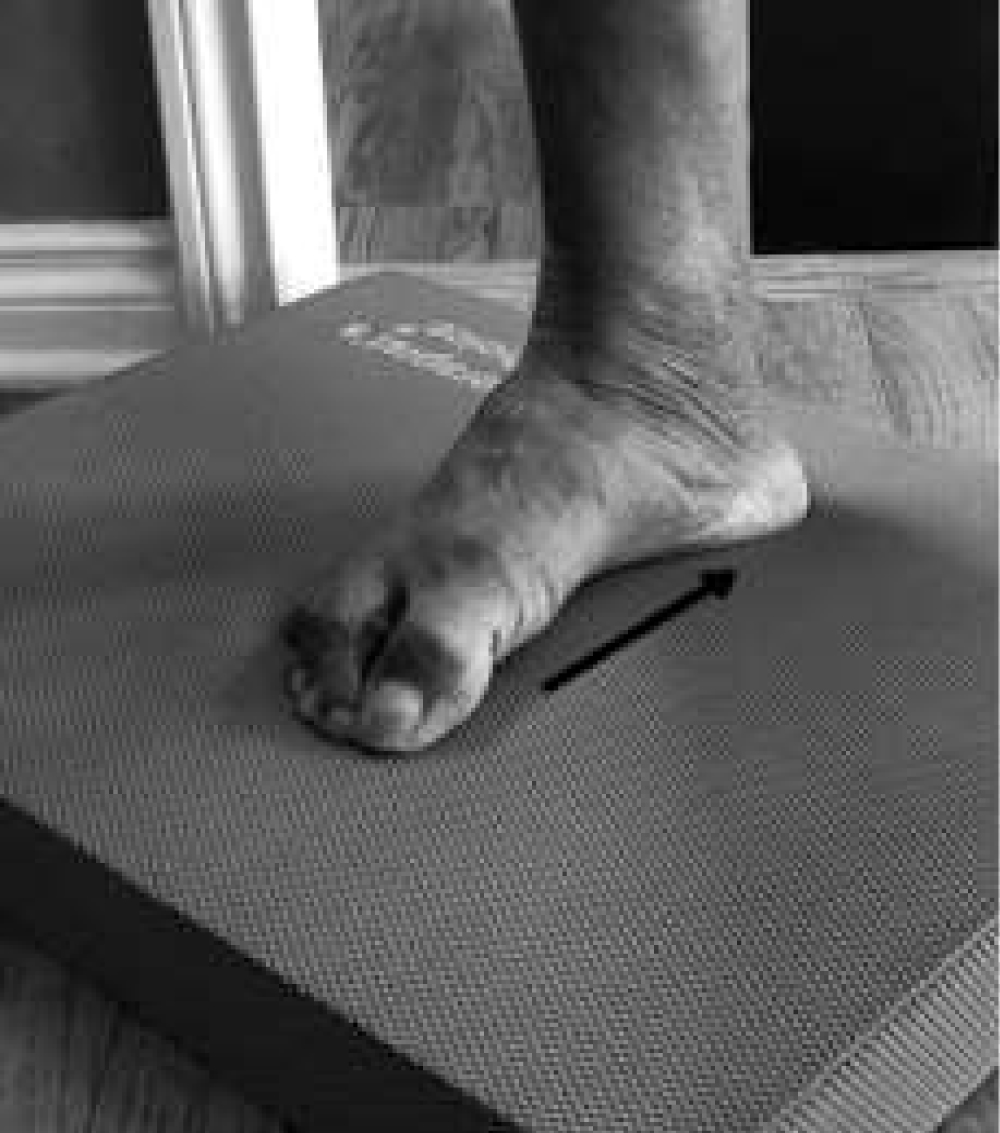 Figure 9: Standing intrinsic training on padded surface.
View Figure 9
Figure 9: Standing intrinsic training on padded surface.
View Figure 9
 Figure 10: Standing unilateral heel raise.
View Figure 10
Figure 10: Standing unilateral heel raise.
View Figure 10
 Figure 11: Standing hip abduction with resistance band.
View Figure 11
Figure 11: Standing hip abduction with resistance band.
View Figure 11
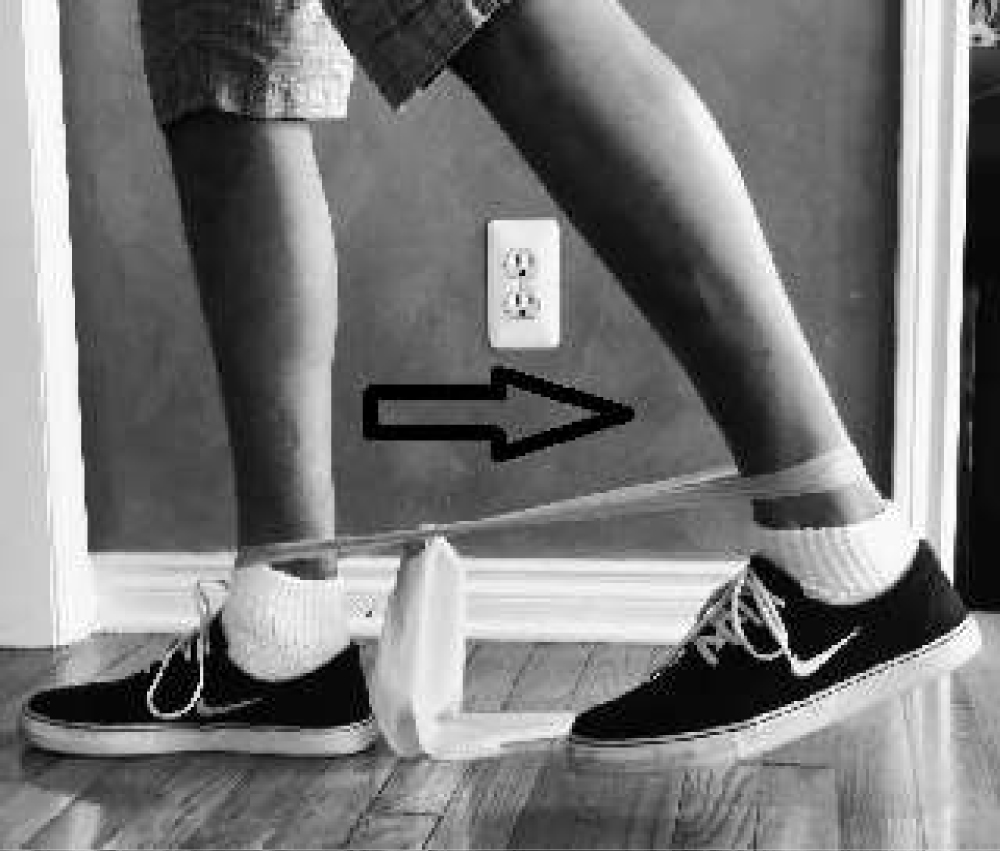 Figure 12: Standing hip extension with resistance band.
View Figure 12
Figure 12: Standing hip extension with resistance band.
View Figure 12
Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11 and Figure 12.
At the end of the fourth week, upon completion of 8 treatment sessions, the following findings were recorded. The patient reported a decrease in the intensity of pain to 2/10 at its worse and 0/10 at best on the NPRS scale with negligible symptom reproduction on local pressure over the shin and calf area. He exhibited improved and full range of motion in passive and active dorsiflexion in supine lying. He reported negligible nighttime pain with twitching on and off. He was functioning with almost no discomfort during routine activities of daily living including his routine walks. He planned to resume running during the springtime. His lower extremity functional scale (LEFS) score was 78/80 and his Global Rating of Change (GROC) score was 5+ (A good deal better). The LEFS and GROC are considered reliable self-report measures for pain and function [50,51]. At the conclusion of the 4-week treatment period a retest of the ASDT was performed. In the standing position with the knees completely extended, the patient was asked to curl his toes inwards to raise the medial longitudinal arch and invert and dorsiflex the foot and ankle. He presented with no difficulty curling his toes and inverting and dorsiflexing the foot. Dorsiflexion range exhibited on the right side was 15 degrees. Passive and active inversion was full and free.
The ankle and foot are made up of 26 bones and divided into 3 regions, the rearfoot, midfoot and forefoot [27]. The well described muscles controlling all movements of the ankle are arranged in compartments in the lower leg [27]. Of interest is the mechanics of the ankle and foot during the gait cycle and the mostly overlooked role of the four layers of intrinsic muscles in the sole of the foot [52].
While the mechanics of the foot during normal gait cycle is reviewed the following speculations can be put forth that may have a clinical relevance to this case report. Chronic pronation has been established as a potential contributing factor for lower leg ankle and foot pain [28,29,19,20,24,25]. The inability of the foot to reverse into supination by increasing the height of the medial longitudinal arch (Figure 13) may be the key component that needs to be addressed, by therapeutic intervention. However, a dynamic test assessing this reversal ability as opposed to a static test that just assesses a navicular drop position or a flattened medial longitudinal arch, may be required. In other words, while a static pronated foot can be identified by observation, observing its dynamic ability to be able to raise the medial arch, invert and supinate may also be of value.
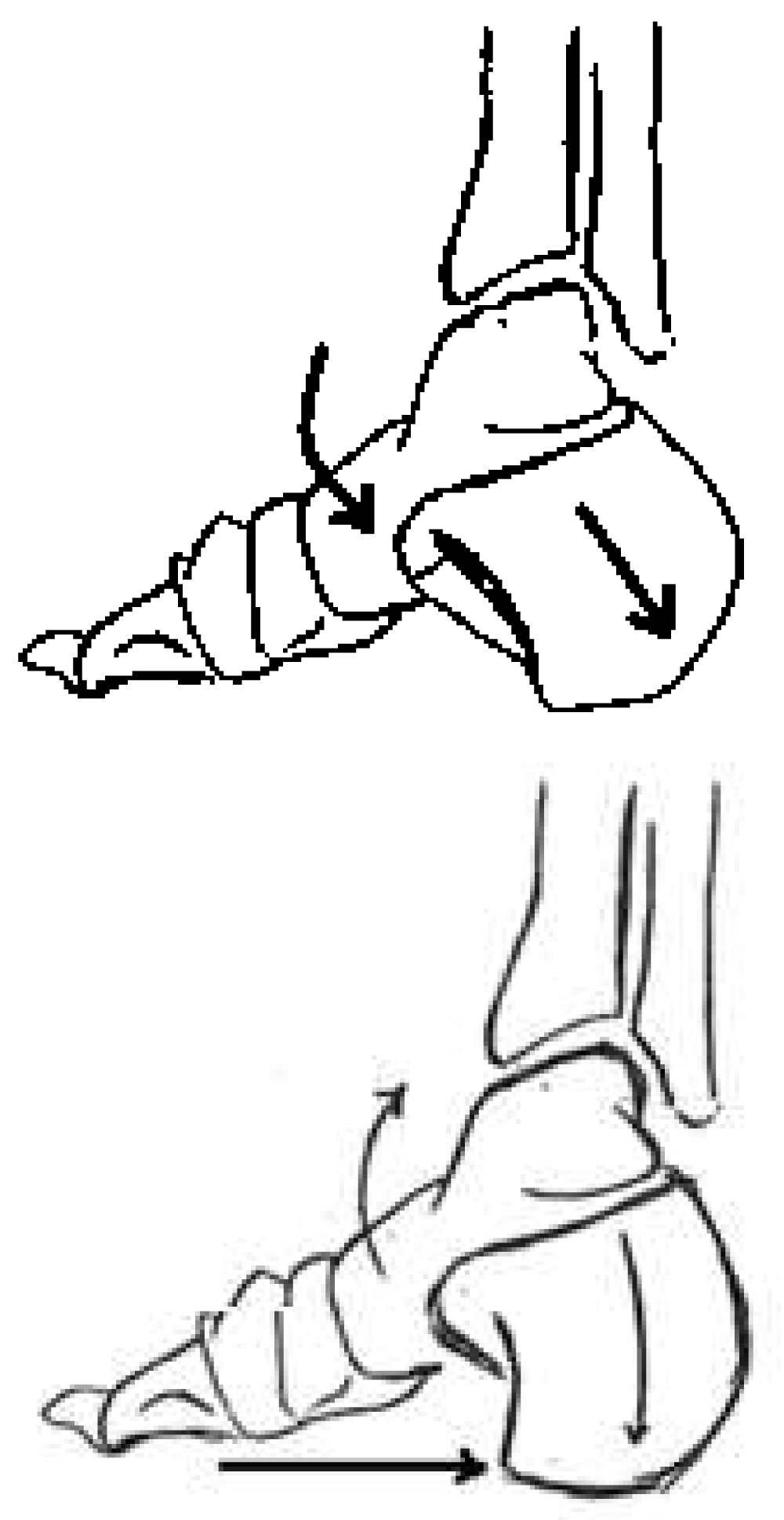 Figure 13: Reversal of pronation to supination during stance phase of gait. (A) Pronation at mid stance; (B) Intrinsic activity combined with supination at late stance.
View Figure 13
Figure 13: Reversal of pronation to supination during stance phase of gait. (A) Pronation at mid stance; (B) Intrinsic activity combined with supination at late stance.
View Figure 13
Pronation is described as a loose packed position that occurs from heel strike to mid and early late stance when there is deformation of the medial longitudinal arch for shock absorption, adaptation of ground terrain changes, and maintenance of equilibrium. In the gait cycle, during heel contact [53,54,27], the talus is described to be in a position of plantarflexion as the foot drops to the ground while being controlled eccentrically by the anterior tibial group. As the foot progresses to mid stance, the eccentrically controlled plantarflexion continues while the talus adducts with calcaneal eversion to drop the medial longitudinal arch. The midtarsal joint, which consists of the talonavicular and the calcaneal cuboid articulations, unlocks with subtalar joint pronation bringing the cuboid and the navicular more parallel. This drops the medial longitudinal arch further, allowing the forefoot to become a loose packed structure [27,53,54]. Additionally, there is an anterior shearing force of the tibia on the talus which is decelerated mainly by the gastrocnemius and soleus muscle groups.
An optimal and timely reversal is hence essential to prevent prolongation of pronation and possible overuse. This is the phase where the lower leg muscles may work in excess if pronation is prolonged, resulting in pain and dysfunction.
At the late phase of stance is when supination begins as it enables the foot to transform into a rigid lever from which to push off. Two aspects are required in a closed chain capacity for supination to be initiated, one being elevation of the loose packed medial longitudinal arch and a more lateral position of the rear foot comprising the talus and the calcaneus [53,54,27]. The literature describes the components of reversal poorly but supports the fact that elevation of the medial arch is assisted and speculated as initiated by the foot intrinsic muscles [55]. The relative dorsiflexion, abduction of the talus combined with calcaneal inversion that follows, creates a more lateral position of the rear foot completing the process of reversal into supination [53-55]. The ASDT aims to identify the ability of a pronated foot to perform this reversal as an active clinical test.
The plantar intrinsic foot muscles play a crucial role in supporting the medial longitudinal arch, providing the foot stability and flexibility required for shock absorption. These muscles also can eccentrically sustain foot pronation for shock absorption and reverse pronation by increasing the height of the medial longitudinal arch during terminal stance [26]. Researchers tested and described that the medial longitudinal arch can deform under increasing load, producing stretch of the plantar intrinsic foot muscles (Abductor Hallucis, Flexor Digitorum Brevis and Quadratus Plantae) and an increase in involuntary activity favoring shock absorption. These muscles were then capable of generating sufficient forces to attenuate medial longitudinal arch deformation produced by the load and reverse the process by effectively increasing medial longitudinal arch stiffness. Activation of these muscles with load and their ability to generate sufficient force to counter medial longitudinal arch deformation may have important implications for how the foot can first absorb and then generate energy for efficient push off during gait [26,45].
While this is a normal process the pathomechanical situation is when this reversal of supination does not occur to a point where push off occurs in a pronated loose packed position. This is what is described dysfunctional pronation and a contributor to multiple pain syndromes in the ankle, foot, and lower leg [20,24,25]. This reversal of pronation and lack thereof is what is targeted mostly during rehabilitation intervention [56]. Chronic fatigue of the decelerators of pronation in the anterior and posterior compartments and the persistent eversion sustained by the lateral compartment [52] are described as the potential mediators of pain in the lower leg.
In conclusion, a chronically pronated foot that poses difficulty with reversal into supination may exhibit the following mechanical challenges. The intrinsic foot muscles do not have the ability to effectively raise the medial longitudinal arch as an initiation of the reversal process. This results in the talus being in a position of chronic plantarflexion and adduction favoring tightness of the gastrocnemius and soleus with subsequent difficulty to dorsiflex the ankle. The ASDT aims to capture this dysfunctional situation by making the individual actively supinate the foot by raising the medial longitudinal arch and performing inversion and dorsiflexion of the ankle in an upright standing posture.
This case report describes a common cause for lower leg pain and the benefits of physical rehabilitation in its management. Prolonged pronation during the stance phase of gait, is described as a causative factor for pain syndromes in the lower leg [20,24,25]. There is anatomical evidence to support the role of the intrinsic muscles of the foot and subtalar mobility, in their ability to reverse pronation to supination during normal gait [53,54,55,27,26]. While a chronically pronated foot has difficulty initiating this reversal process, a novel clinical test to identify this reversal difficulty, has been presented. The test is considered safe with no potential adverse effects. It may be utilized in a screening cluster to identify the presence of dysfunctional pronation. Additionally, it may also be used to assess treatment outcomes. Future research to investigate its diagnostic utility is recommended.