Pseudomonas aeruginosa is one of the most prevalent pathogens in China. However, little is known about the prevalence of clinical P. aeruginosa isolates causing bloodstream infections (BSIs) in China.
BSI-causing P. aeruginosa (BSI-PA) was collected from six tertiary-care hospitals in Beijing. Genetic relatedness was analyzed by pulsed-field gel electrophoresis (PFGE); Antimicrobial susceptibility testing was performed by agar dilution method, and sequence types (STs) were evaluated by multilocus sequence typing (MLST).
A total of 80 non-duplicated BSI-PA isolates were collected from December 2013 to December 2014 and categorized into 69 types (strains) using unique PFGE patterns. Among the 69 BSI-PA strains, 41 STs were identified. Overall, the primary STs were ST244,ST274,ST260 and ST1052 (n = 18), followed by ST270, ST235, ST1295 (n = 3), and ST242, ST275, ST316, ST357 (n = 2). There were 25 STs that only contained a single strain. Approximately 31.9% (22/69) of the strains exhibited carbapenem-resistant phenotype, and most of them carried blaVIM.
The majority of BSI-PA strains exhibited high genetic diversity and low resistance to commonly used antimicrobials.
Molecular epidemiology; Antimicrobial susceptibilities; Bloodstream infections; Pseudomonas aeruginosa
Pseudomonas aeruginosa is one of the most common causes of bloodstream infections (BSIs) in hospitalized patients. BSIs have been considered as a public health problem worldwide. For patients in the intensive care unit, BSIs are the leading healthcare-associated infections, and have been linked to high morbidity and mortality [1]. The mortality rate for P. aeruginosa-induced BSI has been found to be up to 42%, depending on the population studied [2].
The incidence of BSIs caused by multi-drug or pan-drug resistant pathogens is gradually increased in recent decades, it has attracted much attention from many researchers. Some studies revealed that the genetic background of P. aeruginosa is diverse, and the majority of BSI-PA isolates belong to non-clonal population [3].
Recently, 80 non-duplicate BSI-PA isolates were collected from six tertiary-care hospitals in Beijing from December 2013 to December 2014. Antimicrobial susceptibilities and prevalence of carbapenemase genes were detected. The molecular epidemiology was also analyzed.
A retrospective multicentre study focusing on the prevalence of BSIs caused by Gram-negative pathogens was performed in six tertiary-care hospitals located in Beijing, China, including Chinese PLA General Hospital (Hospital A), 302nd Hospital of China (Hospital B), Rocket Army General Hospital, PLA (Hospital C), PLA Army General Hospital (Hospital D), Navy General Hospital, PLA (Hospital E) and Air Force General Hospital, PLA (Hospital F). A total of 80 non-duplicate clinical BSI-PA isolates were collected from December 2013 to December 2014. All clinical isolates were isolated by China-blue agar plate (Thermo Biochemical products [Beijing] Co., Ltd.) and identified by VITEK MS (bioMérieux SA, Marcy- l'Étoile, France). P. aeruginosa ATCC 27853 was used as the quality control strain for antimicrobial susceptibility testing. Salmonella enterica serovar Braenderup strain H9812 was used as a reference standard for pulsed-field gel electrophoresis (PFGE) using CHEF DR-III (Bio-Rad Laboratories). Interpretation of PFGE patterns was performed using the Dice similarity coefficient of BioNumerics software (Applied Maths, St-Martens-Latern, Belgium). Clusters were defined as DNA patterns based on ≥ 70% similarity. The strain with similarity < 5% was considered as the representative of subtypes within the main group. No ethical approval was obtained for using the clinical samples as these samples were collected during routine bacteriological analyses in public hospitals and the data were analyzed anonymously.
Antimicrobial susceptibilities were determined by the agar dilution method. The following antibiotics were tested: piperacillin-tazobactam, ceftazidime, cefepime, cefoperazone-sulbactam, meropenem, imipenem, ciprofloxacin, aztreonam, amikacin. All susceptibility results were interpreted according to the performance standards of the Clinical and Laboratory Standards Institute (CLSI) [4].
PFGE with SpeI was performed for all clinical BSI-PA isolates. The PFGE patterns were analyzed by the Dice similarity coefficient of BioNumerics software (Applied Maths NV, Sint-Martens-Latem, Belgium). Isolates were considered as the same strain (PFGE type) if they possessed the genetic similarity of ≥ 95%. MLST was carried out for all strains according to the protocols available on the MLST websites (http://pubmlst.org/paeruginosa/). STs were clustered into groups by eBURST v3.0 software (http://eburst.mlst.net/) to determine the clonal relationship among the isolates.
Carbapenemase genes, including blaKPC, blaIMP, blaAIM, blaDIM, blaGIM, blaSIM, blaVIM, blaSPM, blaNDM and blaOX-48, were screened for carbapenem-non-susceptible BSI-PA strains as previously described [5].
A total of 857 non-duplicate Gram-negative bacilli isolated from BSIs were collected from six tertiary-care hospitals in Beijing from December 2013 to December 2014. P. aeruginosa accounted for 9.3% (80/857) of all Gram-negative bacilli BSI episodes. Among 80 BSI-PA isolates, 19, 8, 16, 22, 10 and 5 isolates were obtained from hospitals A, B, C, D, E and F respectively.
Isolates with the same PFGE type were considered as the same strain. The 80 non-duplicate BSI-PA isolates were categorized into 69 types (strains) using unique PFGE patterns. Among them, 62 types only had one BSI-PA isolates, five types had 2 BSI-PA isolates, and two types contained four or three BSI-PA isolates, respectively. Therefore, a total of 69 BSI-PA strains without genetic relationship were further analyzed.
Among the 69 BSI-PA strains, 41 STs were identified. Overall, the primary STs were ST244,ST274,ST260 and ST1052 (n = 18), followed by ST270, ST235, ST1295 (n = 3), and ST242, ST275, ST316, ST357 (n = 2). Also, there were 25 STs that contain only a single strain.
Approximately 76.3% and 72.5% of BSI-PA strains exhibited sensitive to meropenem and imipenem, respectively. While 76.3%, 54.4%, 91.3%, 86.5% and 71.3% of strains were sensitive to ceftazidime, cefepime amikacin, ciprofloxacin, aztreonam and piperacillin-tazobactam, respectively. Approximately 34.8% of the strains exhibited carbapenem-resistant phenotype. Most of them produced VIM carbapenemase (Table 1).
Table 1: The characteristics of carbapenem-resistant BSI-PA. View Table 1
P. aeruginosa is one of the leading causes of nosocomial infections and responsible for ∼10% of all hospital-acquired infections worldwide [6]. In addition, P. aeruginosa is responsible for 15.6% of all nosocomial pneumonia cases in medical-surgical ICUs [7]. In China, P. aeruginosa accounts for 19.4% of all isolates in ventilator-associated pneumonia and exhibits a high level of resistance to commonly used clinical antibiotics [8]. In this study, P. aeruginosa was one of the most common pathogens for BSI and accounted for 9.3% of all Gram-negative bacilli BSI episodes. The susceptibility test showed that BSI-PA strains were highly sensitive to ceftazidime, amikacin and ciprofloxacin, which can be the choice for empiric anti-infective therapy.
In this study, 23.7% and 27.5% of BSI-PA strains exhibited resistance to meropenem and imipenem, respectively. Our results are similar to those of P. aeruginosa isolates from hospital-acquired pneumonia in China, but lower than those of isolates from ventilator-associated pneumonia (41.1% and 38.9%, respectively) [8]. Meanwhile, our results are slightly higher than the results from a study from the United States, in which 21.9% and 15.4% of P. aeruginosa isolates were resistant to imipenem and meropenem, respectively [9]. Therefore, it is necessary to raise the awareness of antimicrobial resistance associated with different P. aeruginosa strains because the resistance of P. aeruginosa isolated from different sites of infection or different regions to a given agent could be very diverse. The major mechanisms for the resistance of P. aeruginosa isolates to carbapenems include carbapenemase production, mutations may lead to low permeability of the bacteria outer membrane, and overexpression of efflux pumps [10]. In this study, 66.7% (16 of 24) of carbapenem-resistant strains produced VIM or IMP (Table 1), suggesting that carbapenemase production may play an important role in the carbapenem-resistant phenotype. Interestingly, 18.8% (13/69) of strains exhibited non-susceptible to carbapenems but susceptible to ceftazidime (Table 1). This phenotype is becoming more and more prevalent, constituting 10.1% to 13.5% of PA-BSI strains in many institutions worldwide [11]. Previous studies indicated that some resistance mechanisms may be specific to certain carbapenems, but not to the whole class of beta-lactams [10]. For example, the imipenem-resistant ceftazidime-susceptible isolates showed decreased mRNA expression of oprD, and overexpression of mexB [12], while the loss of OprD and overexpression of mexXY-OprM and mexAB-OprM were associated with carbapenem resistance in cephalosporin-susceptible P. aeruginosa [13]. These results suggested that some mutations may result in decreased expression or absence of outer membrane proteins and overexpression of some efflux pumps target only certain carbapenems, and then lead to the carbapenem-resistant cephalosporin-susceptible phenotype in P. aeruginosa [10]. Thus, clinicians may consider the use of ceftazidime, cefepime, or piperacillin-tazobactam against these P. aeruginosa isolates. Some studies suggested that non-carbapenem-beta-lactams (ceftazidime, piperacillin, and/or piperacillin-tazobactam) may still be effective alternatives for short-course therapy for BSI caused by P. aeruginosa strains, but should be used with caution in high-inoculum infections such as endocarditis and osteomyelitis [11,12].
In this study, PFGE analysis showed that 89.9% (62/69) of clinical BSI-PA isolates had a unique pattern, indicating widespread diversification of BSI-PA strains in this area. The results from other regions also showed similar results [3,14]. The non-clonal population structure of BSI-PA isolates suggests that no clonal transmission of P. aeruginosa between inpatients with BSI, but these patients should be addressed even in the non-outbreak setting. The results also indicate the importance of continuous, consistent surveillance of nosocomial infections in high-risk patients. In addition, the MLST results of BSI-PA showed a genetic background of clone diversity distribution, but no significant clone prevalence (Figure 1). Other studies have reported that the genetic background of P. aeruginosa is diverse [15], which is consistent with the results in this study. Only two small outbreaks of BSI-PA strains occurred, in which ST1052 and ST274 appeared in four and five BSI-PA strains, respectively.
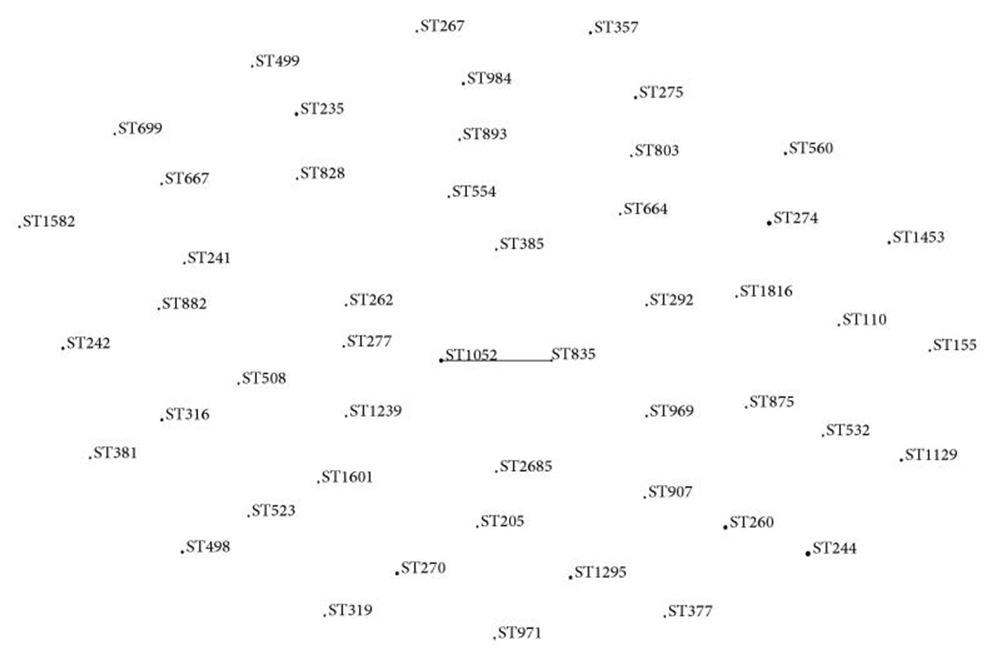 Figure 1: The eBURST diagram of MLST. Lines connect single locus variants. The relative size of the dots indicates the abundance of each ST. View Figure 1
Figure 1: The eBURST diagram of MLST. Lines connect single locus variants. The relative size of the dots indicates the abundance of each ST. View Figure 1
However, the present study has the following limitations. First, the main drawback of the study is the paucity of information on the clinical characterization of patients. Second, the resistance mechanisms other than MBL production, such as the expression of OprD and MexAB-OprM have not been analyzed.
This study was financially supported by the Special Key Project of Biosafety Technologies for the National Major Research & Development Program of China (2017YFC1200803).
The authors have no conflicts of interest to declare.