This study examined integration between local public health agencies and primary care clinics in Nebraska, highlighting progress to date, successes, opportunities, and barriers.
The study included a survey of all 19 Local Health Departments (LHD) directors in Nebraska, and semi-structured follow-up interviews with five LHD directors.
There is considerable evidence of integration activities between primary care clinics and LHDs. Current activities focus on care coordination for high-risk chronic care patients and promoting hypertension, diabetes, and cancer screening. Six LHDs have a formal contract or memorandum of understanding with one or more clinics, and at least two LHDs are embedding nurses within clinics. Although LHDs felt there were many benefits to integration and emerging opportunities, significant barriers persist, including funding, administrative capacity, and data sharing.
Readiness to integrate public health and primary care services varies from one community to the next. Public health and primary care must continue to build partnerships and pilot new integration activities, while state agencies, universities, professional associations, and others must work to address funding and technical barriers. Public and private insurers should encourage clinics to screen patients for major risk factors, particularly social determinants of health, and provide incentives to improve individual and population health outcomes. More funding and technical assistance are needed to enhance integration activities. Future studies should evaluate the costs and benefits of integration projects from both the provider's and the patient's perspective, as well as organizational and systems perspectives.
Local health departments, Primary care, Integrated care, Integrated health system
National and local health systems are in the midst of major transitions, which provide public health and primary care a unique opportunity to build a more integrated system of prevention and treatment. The Institute of Medicine defines integration as, "the linkage of programs and activities to promote overall efficiency and effectiveness and achieve gains in population health" [1]. Integration has become an important priority of health systems because of the shift from fee-for-service to value-based reimbursement and the implementation of new health care delivery models, such as Patient-Centered Medical Homes (PCMHs) and Accountable Care Organizations (ACOs). In addition, health professionals are beginning to recognize how individual health is shaped by social determinants, creating new opportunities for physician clinics to work closely with public health agencies and community-based organizations. If public health and primary care work more closely together, they can align their resources and expertise to reduce the cost of care, prioritize care to those most in need, and improve individual and community health outcomes [1].
Although this study was completed before the arrival of COVID-19, this virus has highlighted the critical need to identify high risk individuals and whenever possible, develop a cohesive prevention strategy. In many areas, COVID-19 has also exposed the fragmentation of the public health and health care systems, the health disparities and inequities of the population, and the negative impact on health outcomes. Both public health agencies and primary care clinics are on the front lines of the COVID-19 crisis. By working together, they have an opportunity to refocus the health system toward keeping individual patients healthy over the long-term and promoting healthy communities.
One of the priority goals of the Nebraska's State Public Health Improvement Plan (SHIP) is to develop an integrated health system that values public health as an essential partner. As part of the SHIP goal, an environmental scan was initiated to examine the integration and linkages of the activities and programs between Nebraska public health agencies and primary care clinics in 2017. This assessment found strong evidence of integration activities between primary care clinics and Local Health Departments (LHDs) in Nebraska [2,3], but rapid changes are occurring in a very dynamic environment. The purpose of this study was to complete a follow up scan to document and highlight changes, successes, and barriers, as well as prospects for the future.
For the first half of the twentieth century, public health and primary care physicians grew apart. In the 1960s, this separation began to close when the Community-Oriented Primary Care (COPC) model became the framework for the community health center movement. Also, the Folsom Report published in 1967 helped to establish the specialty of family practice and encouraged a strong link between primary care and community health service delivery [4]. Until the 2000s, however, population health was not woven into the mainstream of primary care practices. With the adoption of the PCMH and ACO models, population health and the influence of the social determinants of health became an integral part of many practices [4].
Researchers have also begun to study the types of integration models and their impact on patients, organizations, and outcomes. They have found that integration is a broad concept that is aimed at improving service efficiency, patient experience, and outcomes. A recent study concluded that "integrated care is best understood as an emergent set of practices intrinsically shaped by contextual factors and not as a single intervention to achieve predetermined outcomes" [5].
The Rainbow Model of Integrated Care and its taxonomy of 59 key features distributed across six integration dimensions, including clinical, professional, organizational, system, functional, and normative integration was used the theoretical foundation for this study [6,7]. The Rainbow Model of Integrated Care offers a way of understanding how integrated care enables health systems to achieve lower cost and improved care while advancing both individual and population health. Importantly, it details the complex and multidimensional nature of integrated care. The framework allows researchers to evaluate how effectively health systems integrate care at the macro-level (e.g., system integration to include resource availability across partners and health determinants of the population), the meso-level (e.g., organizational and professional integration to include performance management and collective learning between organizations), and the micro-level (e.g., clinical integration to include case management, patient education, and continuity of care). It also includes functional integration (e.g., human, information, and resource management) and normative integration (e.g., visionary leadership and collective attitude that shared vision).
The scan followed the principles of practice-based systems research. These principles involve systematic inquiry into the systems, methods, policies, and programmatic applications of public health practice, with the goal of improving the quality, performance, efficiency, and effectiveness of public health systems that affect community health outcomes [8]. The University of Nebraska Medical Center Institutional Review Board considered this study to be a quality improvement project and declared that it was non-human subject's research.
Nebraska's public health system is regionalized and includes 19 LHDs. Of these 19 LHDs, 16 are multi-county and range in size from two to eleven counties. A total of 15 LHDs are in rural areas and five of them cover mostly frontier areas (less than 6 persons per square mile). All 19 LHD directors responded to a 22-question survey to identify their current integration efforts. The survey covered six topics: (1) Clinical care coordination; (2) Public health programming and prevention; (3) Barriers, benefits, and opportunities; (4) Current resources and support for integration; (5) Common metrics and priorities; and (6) Future needs. The survey was administered via Survey Monkey in June and July 2019.
After the survey, semi-structured interviews were conducted with five LHD directors representing small, medium, and large health departments. The interviews were used to draw interpretations to better understand the results of both [9].
All 19 (100%) of the LHD directors completed the survey. Five LHD directors were interviewed in July to supplement the information gleaned from the survey. Themes that emerged from the surveys and interviews included perceptions of benefits, progress on community health efforts, planning and implementation, opportunities, and barriers.
Overall, survey respondents identified several benefits of working with physician clinics (Figure 1), including reinforcement of messages for behavioral change (84 percent), better health outcomes (79 percent), closing care loops (74 percent), an increase in referrals to their community programs (68 percent), an increase in collaboration with community-based physician extenders, such as pharmacists (58 percent), and reduced duplication of services (47 percent).
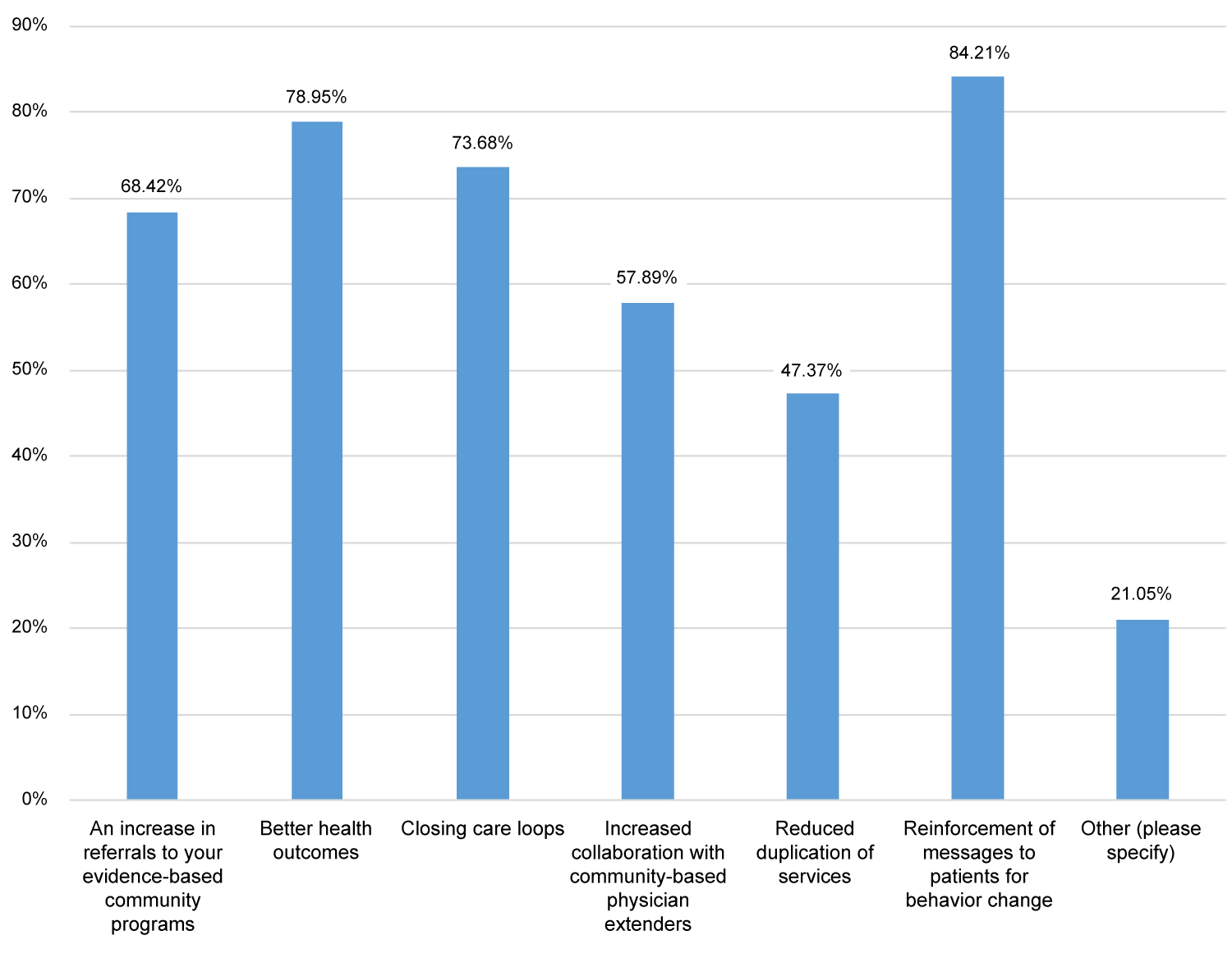 Figure 1: What are the primary benefits your LHD is gaining by working with physician clinics?
View Figure 1
Figure 1: What are the primary benefits your LHD is gaining by working with physician clinics?
View Figure 1
Interviews revealed additional perceived benefits of integration. One of the major benefits is being able to target the social determinants of health, which has the potential to improve population health outcomes in their communities. Other benefits were building stronger relationships with clinics, breaking down cultural and social barriers, and improving awareness of community resources. According to one LHD director, "When we work together, we are able to build relationships that help us define gaps and build capacity in our communities." Another LHD director noted that integration will lead to "healthier people and better quality of life. The reason that we exist is to make the public healthier and safer and I believe this is the right thing to do. It aligns with our mission and purpose just perfectly."
Respondents were asked to report on their screening activities for pre-diabetes and hypertension from July 1, 2018 to June 30, 2019. Eight LHDs offer a pre-diabetes screening program (e.g., the National Diabetes Prevention Program), and 204 people were screened over the one-year period. In addition to screening for prediabetes, 14 LHDs provided hypertension screening to over 2,200 people, 16% of whom were referred to physician clinics for follow up treatment.
Of the 18 respondents that answered the question about cancer screening, all indicated that they promote cancer screening through a variety of venues, including through social media (100 percent), and traditional media, health fairs, and health coaching (78 percent). In addition, 83 percent distributed fecal occult blood test kits during the one-year period, and at least 25 people with abnormal readings were referred to a physician for follow-up.
When asked about vaccinations for children and adults, 17 respondents indicated that they provide them. Of those who do, 76 percent reported they have a strong partnership with physician clinics in their jurisdiction.
Ten respondents indicated that they engaged in worksite wellness activities in the past year. All 10 provided health education for high-risk behaviors, and 70 percent provided screening for diabetes, hypertension, and cholesterol. Sixty percent of the LHDs administered a health risk assessment for employees and provided technical assistance for policy changes (e.g., offering more nutritious options in company vending machines). One LHD director described a new partnership that involves the LHD, the physician's clinic, and the hospital to work with a large employer. The role of the LHD is to conduct a health risk appraisal for all employees, identify high-risk factors, and develop strategies (e.g., nutrition and physical activity programs) to improve the health of employees. The clinic is responsible for providing health screenings (e.g., diabetes and hypertension) and referring employees with abnormal rates for follow-up care. The hospital assesses occupational risks and does an ergonomic and body fat analysis.
Almost 90 percent of the LHDs employ Community Health Workers (CHWs) to connect clients with community health-related services and resources. Most LHDs (53 percent) employ between three and four CHWs. In terms of CHW functions and activities, almost all LHDs (84 percent) use CHWs to connect clients to community programs and resources and 63 percent have them provide health coaching to change unhealthy behaviors and for translation and interpretation. CHWs are also involved in a variety of other tasks, such as screening for diabetes and hypertension, assisting clients enrolling in Medicaid and exchange insurance plans, conducting home visits, providing medication management assistance, and working closely with PCMH care coordinators (Figure 2).
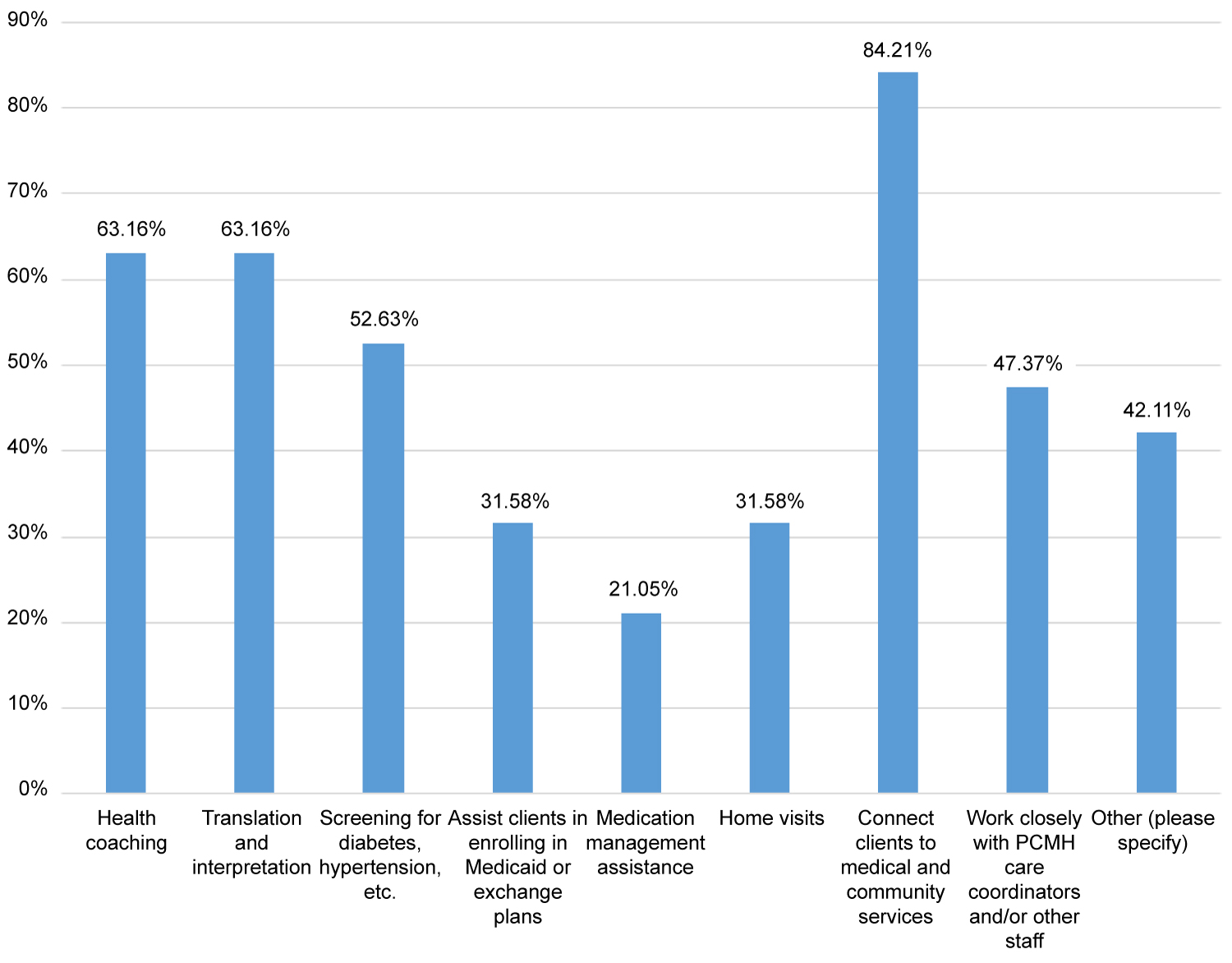 Figure 2: If you employ CHWs, what are their functions and activities?
View Figure 2
Figure 2: If you employ CHWs, what are their functions and activities?
View Figure 2
Six LHDs (32 percent) have formal agreements (e.g., a contract or an MOU) with one or more physician clinics. Some have developed new models of integration that may prove to be a key opportunity for other LHDs. For example, in one LHD a nurse recently began working part-time in a physician's clinic to coordinate care for high-risk patients, including assuring medication compliance, scheduling follow-up visits, screening for social determinants such as food and housing security, and linking patients to LHD and other community-based programs and activities (e.g., diabetes prevention and tobacco control programs). To satisfy HIPAA requirements, data sharing occurs through a business associate agreement. To fund this project, the clinic is proposing using additional funds from the CPC+ program; a portion of the funds will be retained by the clinic to cover administrative expenses, while the remaining funds will be used to pay for the nurse. Another LHD is sharing a CHW with a primary care clinic. The CHW is responsible for linking high-risk chronic care patients from the clinic with LHD and community-based programs, and contacts patients about medication compliance and follow-up visits with the clinic. A third LHD is contracting with a FQHC to embed a nurse from the LHD in the clinic. Initially, the nurse will be responsible for monitoring ten of the most complex, high-risk patients, including at least one home visit, screening for social determinants of health, and referral to LHD and community-based programs. Data will be shared through a business associate agreement, and the FQHC will pay for the nurse's time through the Medicare Chronic Care Management Program. If the model is successful, it will be expanded to other patients.
LHDs also partner with physician clinics other ways (Figure 3). For example, almost 80 percent provide education to clinic staff about emerging diseases (e.g., Zika virus); 53 percent assist physician clinics in developing referral policies for community services and building relationships with team extenders such as pharmacists; 47 percent develop educational messages for clinic patients; 42 percent connect low-income clients with medication assistance programs; 21 percent conduct home visits for children, assist clinics in analyzing EMR data, and develop quality improvement policies and procedures; and 11 percent coordinate behavioral health services and review clinic materials for health literacy.
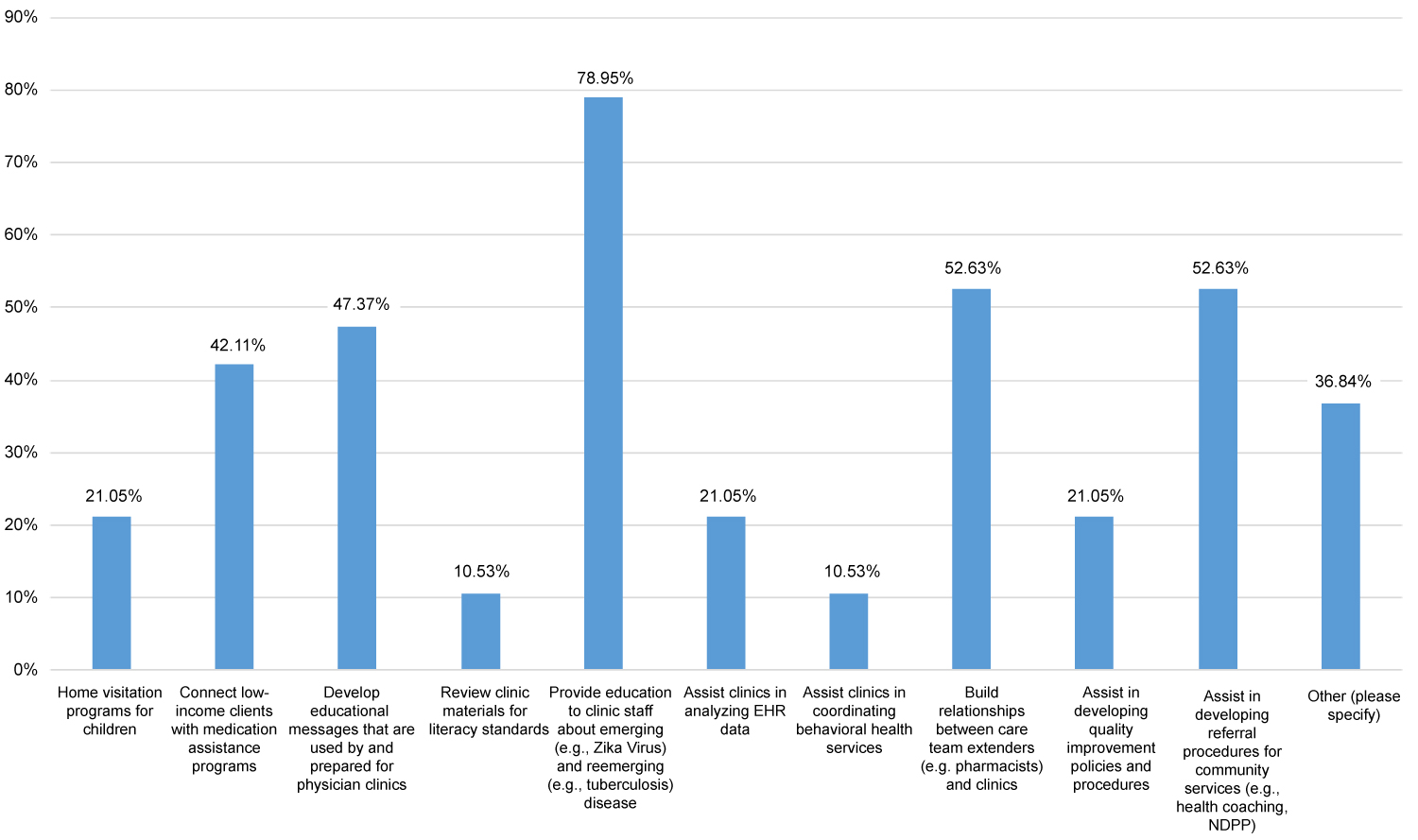 Figure 3: Is your LHD involved in the following programs or activities with physician clinics?
View Figure 3
Figure 3: Is your LHD involved in the following programs or activities with physician clinics?
View Figure 3
When asked about future opportunities for linkages with physician clinics, 79 percent of respondents identified chronic disease health coaching (Figure 4). Other opportunities included lead screening (68 percent), the development of evidence-based policies (63 percent), mental health and substance use coordination (58 percent), dental health services (58 percent), and prevention of opioid abuse (53 percent). LHDs also identified chronic disease management, prevention of falls, care coordination, and transitional care or post-ER follow-up.
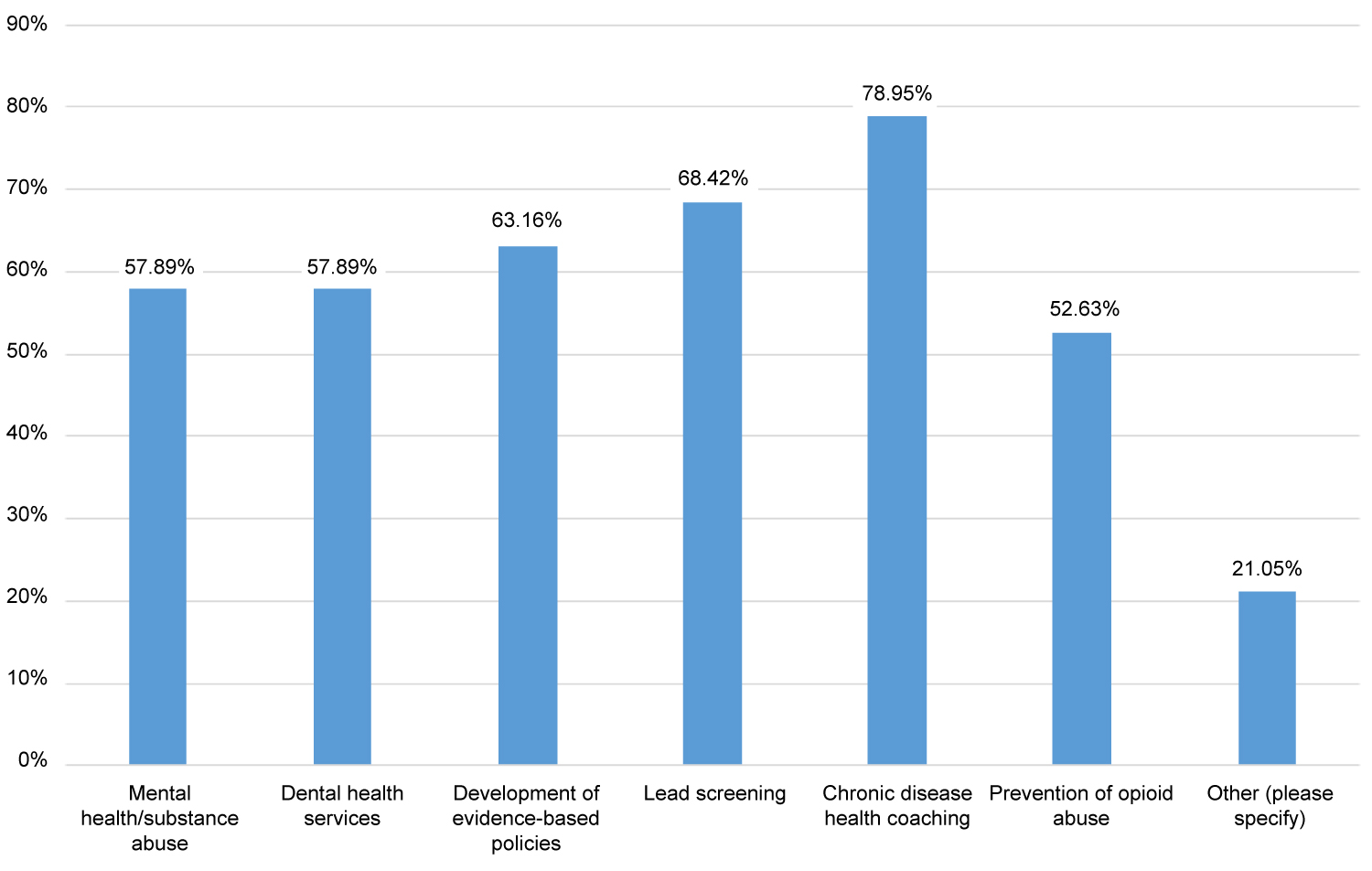 Figure 4: What do you feel are new opportunities for linkages between your LHD and physician clinics in your district?
View Figure 4
Figure 4: What do you feel are new opportunities for linkages between your LHD and physician clinics in your district?
View Figure 4
Interviews revealed additional opportunities for future integration. For example, one LHD is working with local EMS rescue squads to establish better relationships with EMTs so that patients who are frequently transported to hospital emergency departments can be linked to community programs or CHWs to better manage their chronic conditions. Another LHD is assessing current behavioral health practices in clinics to promote evidence-based practices that have worked well in other communities. In addition, several LHDs are working with clinics on fall prevention and getting more patients referred into programs such as Tai Chi. One LHD has also initiated a breast cancer navigation screening program to follow up with women who have not received a mammogram in a timely manner. Finally, one LHD is developing a rural agricultural safety program where CHWs conduct health risk assessments and refer high-risk individuals to physician clinics.
Several barriers were identified that have limited linkage activities between LHDs and primary care clinics (Figure 5), primary among them a lack of funding (84 percent). Currently, most LHDs are funding linkage projects with one or more grants from the Nebraska Department of Health and Human Services. When asked how linkage projects would be funded in the future, most LHDs felt that grant funding would be the most likely source in the future, followed up by Medicaid reimbursement, private insurance reimbursement, and program-generated funds.
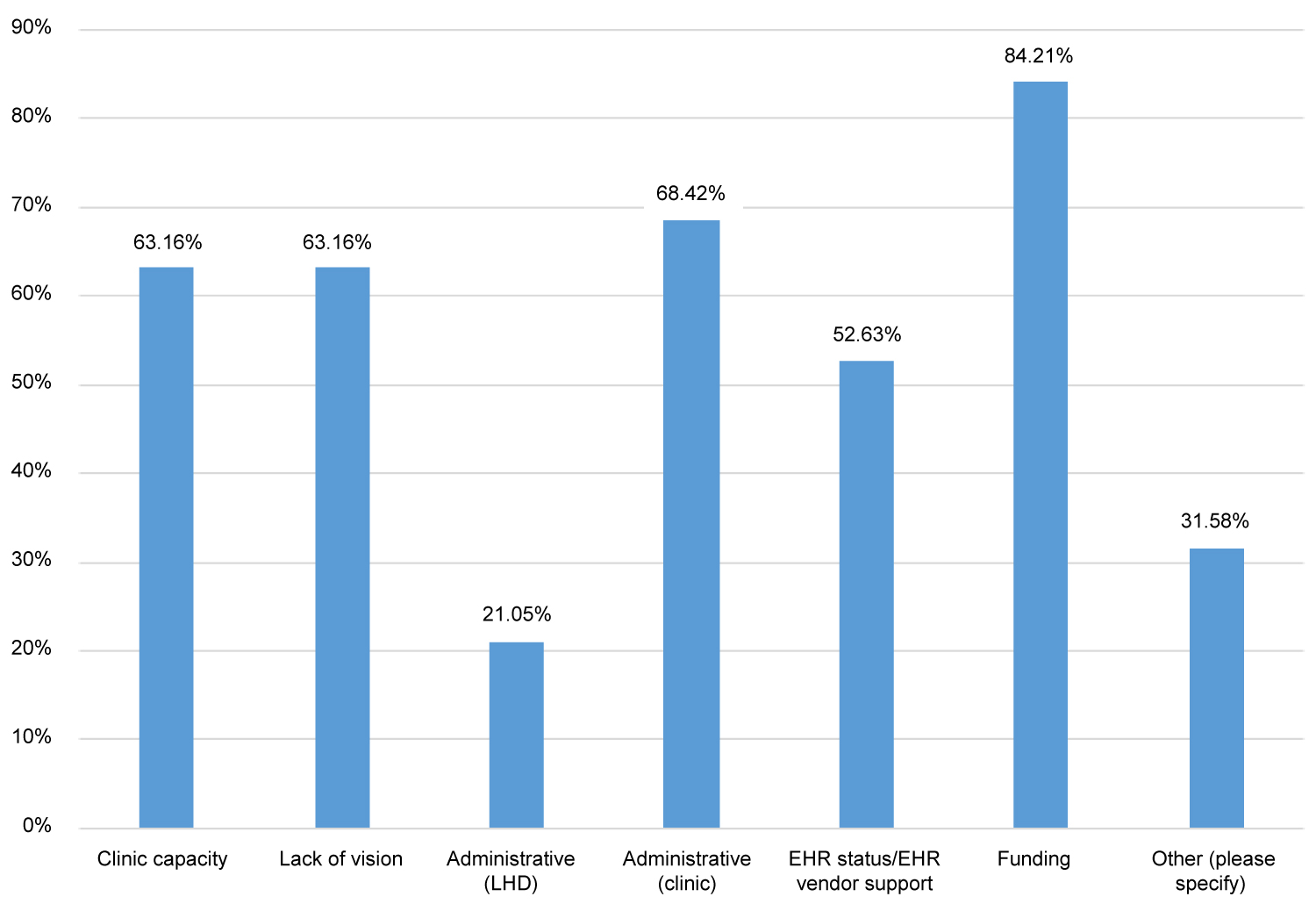 Figure 5: What are some of the barriers that you face when working with clinics?
View Figure 5
Figure 5: What are some of the barriers that you face when working with clinics?
View Figure 5
Additional barriers include administrative capacity in clinics (63 percent), limited clinic capacity (68 percent), lack of vision (63 percent), incompatibility between electronic medical record systems (53 percent), and administrative capacity of LHDs (21 percent).
Interviews revealed additional barriers. For example, training for LHD staff is needed to make these linkage activities more effective. In some cases, there is a cultural divide between clinics and LHDs (e.g., treatment versus prevention). Another barrier is the time and energy it takes to plan and implement these programs. In some instances, both clinic and LHD staffs are "stretched beyond their limits." Turnover of key staff, especially at the leadership level, stalls progress as new relationships and trust must be rebuilt.
Nearly all LHDs play a significant role in helping nonprofit hospitals develop their Community Health Needs Assessments (CHNAs) and implementation plans. When asked how their CHIP priorities compared with CHNA priorities, 63 percent of respondents indicated they were the same or almost identical, while 37 percent reported that about half of their priorities were the same. In interviews, LHD directors agreed that their priorities aligned closely or were identical to the priorities in the CHNAs. One LHD director indicated that one of its CHIP priorities was to explore how community partners could work together to improve care coordination. Another LHD director reported that the priorities in the CHIP are the same as the CHNAs of the nonprofit hospitals. They also have hospital representatives on their planning and implementation committees, so these representatives were involved in the development of the implementation strategies. When asked how aligned implementation efforts are between the LHDs and the nonprofit hospitals, only 37 percent believed their implementation efforts were closely matched and cohesive with the efforts of nonprofit hospitals. In contrast, 53 percent of LHDs indicated they were somewhat matched but not cohesive, and 11 percent of LHDs felt their implementation efforts were not closely matched.
This environmental scan reveals that Nebraska continues to make progress toward an integrated health system that values public health as an essential partner. Reflecting on Valentin, et al.'s taxonomy of integrated care, progress toward integration appears to have sustained primarily along the micro-level (e.g., case management, patient education, continuity of care). Some evidence points to emerging functional integration, particularly as processes and agreements begin to be formalized for human resource management, information management, and resource management. Much less integration has occurred at the meso- and macro-levels, which is further reflected in the lack of normative integration.
Specifically, most linkage activities between LHDs and primary care clinics and hospitals focus on chronic diseases and associated risk factors. Many of these activities involve screening for diabetes, hypertension, and cancer. LHDs are using CHWs as health coaches and linking high-risk patients to community programs and resources. Because of the many perceived benefits from linkage programs, most LHDs continue to work very closely with at least some of their physician clinics.
Although some barriers persist (e.g., funding, administrative capacity, data sharing), many physician clinics, particularly those with a PCMH or ACO designation, now realize that improving individual health also requires improvements in community and population health [1]. As a result, opportunities abound for more linkage projects in the future. For example, six LHDs have a formal contract or MOU with one or more physician clinics, and at least two LHDs either have or plan to embed one of their nurses within a clinic. While specific roles and financing still need to be finalized, these nurses will be able to coordinate care across programs and activities in the community and in the clinic. These steps are important to realize functional integration upon which other integrated care efforts often depend.
During the past year, integration efforts between physician clinics, hospitals, and LHDs have expanded and the potential for new opportunities is growing. Because more physician clinics have transitioned or are transitioning to PCMHs and ACOs, there is considerable momentum for new integration efforts, but there is a lack of system-level leadership to coordinate broader efforts. To capitalize on this momentum, state agencies, universities, professional associations, and others must work to assure the availability of adequate funding and to provide targeted technical assistance. At the local level, the most important priority is to develop effective partnerships between LHDs and physician clinics and hospitals. While LHDs have limited financial resources, they have other assets, including strong relationships with many other community organizations and the knowledge and capacity to bring partners together. Building healthy communities will require a collective vision and leadership from the health care and public health sectors to advance this vision.
Although this study is unique to Nebraska, many of the findings can be generalized to other states, particularly those with sparse populations and large rural areas. Because many of these areas have a shortage of health professionals, older populations with multiple chronic conditions, and limited resources to address the social determinants of health, it is critical for LHDs and primary care clinics to maximize their resources to keep individuals healthy and promote healthy communities. The COVID-19 experience has demonstrated that public health and health care can work closely together, and these partnerships need to be expanded in the post COVID-19 era.
Integration readiness among physician clinics and LHDs varies considerably from one community to the next, and a one-size-fits-all approach is neither feasible nor desirable. To achieve and sustain clinical integration, more investment and coordination should focus on improving the patient experience, enhancing the satisfaction of health professionals, building organizational capacity and financial stability, and improving individual and population health outcomes. For example, public and private insurers can encourage physician clinics to screen patients for major risk factors, particularly social determinants of health, and provide financial incentives to improve individual treatment and population health outcomes. Medicare-funded programs, such as the Medicare Shared Savings Program for ACOs, the Chronic Care Management Program, and Comprehensive Primary Care Plus (CPC+), have provided these incentives and some funding to build infrastructure components. Other funding is also needed from state Medicaid programs and private insurers. This funding should provide incentives for care coordination (e.g., screening all patients for clinical, behavioral risk factors, and the social determinants of health, referrals to LHDs for tobacco cessation and other appropriate programs such as food insecurity, and data sharing).Finally, a state agency or university should be responsible for coordinating integration activities across of its dimensions (the macro-, meso-, and micro-levels).
Future studies should evaluate integration projects and compute the costs and benefits of these projects. Furthermore, studies, including surveys and interviews, should be conducted periodically to capture new integration tools and strategies so they can be shared with others. Studies should also be expanded to include the perceptions of primary care physicians and hospital staff.
This project was funded by the Office of Community Health and Performance Management in the Nebraska Department of Health and Human Services. The authors would also like to thank Augusta Kamara, MPH, for her valuable assistance in helping to collect the data for this project.
The authors have no conflicts of interest to declare.