Examine differences in the associations between core Electronic Health Record (EHR) functionalities for public and population health, care coordination, patient engagement, and quality improvement on the provision of recommended Cardiovascular Disease (CVD) preventive health services provided at Primary Care Visits (PCVs) for CVD at-risk adults with Medicaid and those with private insurance.
Utilizing a nationally representative survey of ambulatory care visits by patients at risk for CVD in 2014 and 2015, binary logistic regression models examined the associations between core EHR functionalities and the provision of recommended CVD preventive services for Medicaid and private insurance patients at risk for CVD, controlling for patient and provider confounding variables.
Primary care providers caring for Medicaid patients were significantly less likely to adopt fully functional certified EHR technology compared to PCPs caring for private insurance patients (75% vs. 82%, p < 0.01). Medicaid patients were significantly less likely to receive recommended blood pressure screening compared to private insurance patients (95% CI, 0.205-0.931). Among preventive visits for Medicaid patients at risk for CVD, significant associations were found between select recommended CVD preventive services and public and population health management, care coordination, and patient engagement.
Mixed results were found between core EHR functionalities and the provision of recommended CVD preventive services provided at PCVs for Medicaid patients. Low physician adoption of fully functional certified EHR technology may have impacted the provision of recommended CVD preventive services for Medicaid patients.
Study findings demonstrate concerns about the rates of recommended CVD preventive services at PCVs for Medicaid patients at risk for CVD, which imply gaps in their care. Further investigation is required to understand how the approved list of electronic clinical quality measures impacts the associations between core EHR functionalities and the provision of recommended CVD preventive services delivered at PCVs.
Population health, Cardiovascular disease, Health information technology, Electronic health records, Primary care
CVD: Cardiovascular Disease; CMS: Centers for Medicare and Medicaid Services; CEHRT: Certified EHR Technology; HER: Electronic Health Record; eCQM: Electronic Clinical Quality Measures; NAMCS: National Ambulatory Medical Care Survey; PCVs: Primary Care Visits
More than 17.3 million people die from Cardiovascular Disease (CVD) in a given year [1]. Hypertension, hyperlipidemia, diabetes, and obesity are preventable risk factors for CVD [2]. Preventable CVD disproportionately affects low-income Medicaid eligible populations [3]. Preventive care, such as blood pressure screening and obesity counseling, is essential to reducing the risk of CVD [4,5]. Low-income Medicaid eligible patients are less likely to receive recommended preventive care compared to higher-income patients with private health insurance [6].
Electronic Health Record (EHR) use has been proven to increase the likelihood of receiving recommended primary preventive care for CVD [7]. Several studies have shown that EHRs integrated with Clinical Decision Support (CDS) functions help physicians to use alerts, reminders, and shared health information to proactively prevent chronic conditions in high-risk safety net patients [8-10]. Despite these important findings highlighting EHRs role in preventing chronic diseases in high-risk patients, the literature remains mixed on whether EHRs can be instrumental in improving CVD outcomes [11,12].
The American Recovery and Reinvestment Act of 2009 set forth the Medicaid EHR Incentive Program, which rewards eligible clinicians who adopt and meaningfully use Certified EHR Technology (CEHRT) to meet a defined set of objectives and measures across three stages. Domain objectives and measures for the advanced use of CEHRT by clinicians include the following core EHR functionality areas: public and population health management; care coordination; patient engagement; and quality improvement [13-15].
Furthermore, electronic Clinical Quality Measures (eCQM) are used by Centers for Medicare and Medicaid Services (CMS) to assess whether eligible professionals, i.e. physicians, are demonstrating "meaningful use" under the Medicaid EHR Incentive Program [16]. The defined list of eCQMs focus on prevalent health conditions that contribute to high rates of morbidity and mortality among most Medicaid beneficiaries and reflect best practices for care delivery [16].
Utilizing the National Ambulatory Medical Care Survey (NAMCS), the purpose of this study is to examine differences in the associations between the presence of core EHR functionalities for public and population health management, care coordination, patient engagement, and quality improvement on the provision of CVD preventive health services provided at Primary Care Visits (PCVs) for nonelderly adults with Medicaid and those with private insurance at risk for CVD, controlling for covariates. By exploring the association that core EHR functionalities has on the preventive care services of PCVs, this research provides new insights on the existing health care delivery processes in primary care settings, the utilization of EHRs to assist with preventing chronic diseases, access to care among vulnerable populations, and quality of care differences across payers. This research further explores the role EHR policy has in chronic disease prevention among Medicaid beneficiaries.
The NAMCS is a nationally representative survey of office-based visits to non-federal ambulatory health care providers involved in direct patient care [17]. Two years of the retrospective nonexperimental publicly available data (for 2014 and 2015) from NAMCS was pooled for the cross-sectional analysis. Further information regarding NAMCS survey instruments, sample design, data collection and processing, and reliability estimates can be found online [17].
Analysis focused on 490 Medicaid nonelderly adults and 3325 private health insurance nonelderly adults ages 18-64 at risk for CVD with a PCV between 2014 and 2015. The difference reflects the fact that the population of Medicaid patients was lower than that of private pay patients in the United States during this period of time [18,19]. At risk for CVD was defined as diagnosed with hypertension, hyperlipidemia, diabetes, or obesity, or any combinations of these diagnoses. Patients with a previous diagnosis of cerebrovascular disease, congestive heart failure, or ischemic heart disease, and women who were pregnant were excluded.
Identification of select CVD preventive measures were defined according to the United States Preventive Services Task Force (USPSTF) cardiovascular disorders recommendations for primary care practice and the Centers for Disease Control and Prevention, National Business Group on Health and the Agency for Healthcare Research and Quality's 2006 publication entitled A Purchaser's Guide to Clinical Preventive Services: Moving Science into Coverage [20,21].
The NAMCS contains six outcomes of interest to estimate physicians' use of EHRs to perform recommended CVD preventive services at PCVs. The CVD preventive services of interest pertain to diagnostic/screening services, vital signs, and health education. The first outcome variable measured whether the patient received recommended diet and nutritional counseling, including general dietary guidelines. The next dependent variable assessed whether physicians provided exercise counseling related to the patient's physical conditioning or fitness. The third outcome variable measured whether the patient received recommended counseling for obesity to assist with weight reduction. Analysis assessed whether the patient received blood pressure screening for hypertension. Additionally, analysis estimated whether the patient received lipids/cholesterol screening for hyperlipidemia. The final outcome variable assessed whether the patient received hemoglobin A1c test to screen for diabetes, a well reported risk factor associated with CVD [2].
A stand-alone variable assessed overall physician adoption of CEHRT. Based on the provider's response the following three levels were used to categorize adoption of CEHRT: yes, all electronic; yes, part paper and part electronic; and no. Dichotomous variables ("Yes" or "No") were created for each independent variable of interest indicating whether a physician adopts and meaningfully uses the select core EHR functionality component.
Three variables measured the use of an EHR for public and population health management. The first attribute measured whether the physician generated a list of patients by diagnosis. The second characteristic in this category assessed whether the physician generated a list of patients due for preventive or follow-up care. The final attribute measured whether electronic reminders for guideline-based patient interventions and/or screening test were generated.
Three variables assessed the use of an EHR for patient engagement. The first variable measured whether physicians provided patients with clinical summaries. The second characteristic measured whether physicians provide patients with electronic copies of their health information. The final attribute assessed whether physicians exchange secure electronic messages with patients.
The use of an EHR for care coordination was measured by two attributes. The first variable assessed whether physicians share health information electronically with other providers when referring patients. The second characteristic in this category measured whether physicians receive health information electronically from providers outside their office or group when they refer out a patient, when a patient is referred to them, or when their patient is discharged from an inpatient setting.
The use of an EHR for quality improvement functions was measured by assessing whether physicians reported clinical quality measures electronically to federal or state agencies (such as CMS or Medicaid).
Bivariate descriptive analysis and Wald Chi-Square test were employed to measure patient and provider characteristics, and to assess the relationship between the presence of core EHR functionalities and CVD preventive services provided at PCVs for Medicaid patients and private insurance patients in years 2014 and 2015, respectively. Associations between core EHR functions and primary care content of PCVs for adults with Medicaid and private insurance, controlling for patient and provider characteristics, were expressed as Odds Ratios (OR) from binary logistic regression models. To test whether the effects of core EHR functionalities were independent of insurance status, domain analysis was used to construct subpopulation binary logistic regressions to examine the association between presence of core EHR functionalities and provision of each CVD preventive health services provided at PCVs for Medicaid or private insurance patients, controlling for covariates. Controlled differences were based on patient race and ethnicity, age, and gender. Provider characteristics included physician specialty, type of office setting, type of medical practice, practice ownership, and metropolitan status.
All analysis was computed using SAS version 9.4. All models used NAMCS sampling weights to adjust for the complex sampling design, reduce nonresponse bias, and to ensure a nationally representative sample. This study was exempt from the Institutional Review Board.
Of the 3815 patients at risk for CVD, the mean age for Medicaid patients was 46.8 years and 51.0 years for private insurance patients (Table 1). Patients were similar on characteristics of age, gender, and race/ethnicity. Approximately 75% of PCVs by CVD at-risk Medicaid patients were to a provider who had adopted fully functional CEHRT, compared to 82% of PCVs by adults at risk for CVD with private insurance (p < 0.01). Medicaid PCPs caring for CVD at-risk patients were significantly less likely to generate a list of patients by diagnosis, compared to private insurance PCPs. Furthermore, among preventive visits, those providers caring for Medicaid patients were significantly less likely to provide patients with clinical summaries for their visits and exchange secure messages with patients, compared to providers caring for private insurance patients (p < 0.05). Medicaid PCPs were significantly less likely to conduct care coordination functions compared to private health insurance PCPs.
Table 1: Characteristics of primary care visits for at risk CVD adults 18-64 with Medicaid or Private Insurance, 2014-2015. View Table 1
Overall Medicaid and private insurance patients, respectively, had low rates of diet/nutrition counseling (35.3% vs. 26.9%), exercise counseling (17.8% vs. 18.8%), hemoglobin A1c test (17.9% vs. 8.2%), lipids/cholesterol screening (34.2% vs. 33.1%), and weight reduction counseling (13% vs. 9.6%). An estimated 93.1 percent of visits by adults with Medicaid included blood pressure screening, compared to 96.7 percent of visits by privately insured adults. The results for blood pressure screening, glucose testing, and exercise counseling were statistically significant (Figure 1).
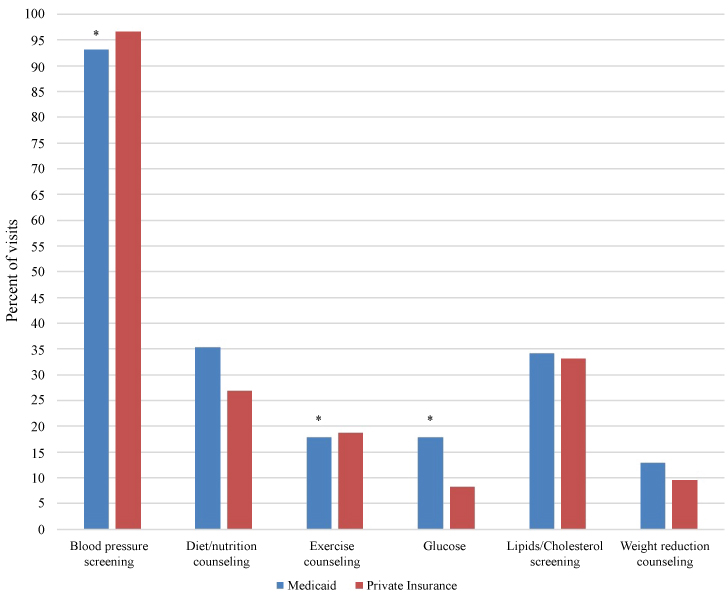 Figure 1: Recommended cardiovascular disease preventive care services of visits to primary care physicians by high-risk adults 18-64 with Medicaid or Private Insurance, 2014-2015. View Figure 1
Figure 1: Recommended cardiovascular disease preventive care services of visits to primary care physicians by high-risk adults 18-64 with Medicaid or Private Insurance, 2014-2015. View Figure 1
Table 2 present descriptive results between overall EHR functionality and CVD preventive services provided at PCVs for Medicaid patients and private insurance patients. Approximately 97% of providers who adopted a fully functional CEHRT completed blood pressure screening on CVD at risk adults. Exercise counseling was rendered by 19% of PCPs who adopted a fully functional CEHRT, compared to 30% of PCPs who conducted exercise counseling with no EHR. These results of exercise counseling were statistically significant. Furthermore, notwithstanding blood pressure screening, overall fully functional CEHRT did not have a large impact on the rates of recommended preventive care.
Table 2: Characteristics of EHR functionality on recommended CVD preventive care services of visits to primary care physicians by at-risk adults 18-64 with Medicaid or Private Insurance, 2014-2015. View Table 2
To determine whether there were disparities in the preventive services offered to patients at risk for CVD and the role health IT has in increasing the probability of receiving recommended primary preventive care for CVD, analysis examined the association between insurance status and core EHR functionalities on the likelihood of services reported as provided. When controlling for patient and provider characteristics, Medicaid patients were significantly less likely to receive recommended blood pressure screening compared to private insurance patients (Table 3). Medicaid patients were less likely to receive recommended exercise counseling and lipids/cholesterol screening, but more likely to receive diet/nutrition counseling, glucose testing, and weight reduction counseling compared to private insurance patients, although these results for health insurance type were not statistically significant.
Table 3: Results from binary logistic regression showing the effect of health IT core functions on primary care content of primary care visits for adults with Medicaid or Private Insurance, 2014-2015. View Table 3
To capture separate effects of core EHR functionalities on health insurance status, separate binary logistic regression analysis was conducted for subpopulations (Table 4). The likelihood of exercise counseling was 92% significantly less for at-risk Medicaid CVD patients whose provider adopted fully functional CEHRT. Furthermore, the odds of at-risk Medicaid CVD patients receiving recommended weight reduction counseling were significantly higher if their doctor generated a list of patients by diagnosis compared to doctors who did not (OR = 6.034, 95% CI = 1.016, 35.828). Glucose level determination was significantly associated with physicians who generated a list of Medicaid patients due for preventive care or follow-up. Medicaid patients at risk for CVD whose doctor sent electronic health information to other providers were approximately 3.1 times significantly more likely to receive exercise counseling compared to Medicaid patients at risk for CVD whose doctor did not send clinical information to other clinicians.
Table 4: Separate binary logistic regression showing the effect of health IT core functions on primary care content of primary care visits for adults with Medicaid, 2014-2015. View Table 4
Significant differences emerged in the provision of clinical preventive services provided to Medicaid patients at risk for CVD versus private insurance patients at risk for CVD. Specifically, Medicaid patients were less likely to receive recommended blood pressure screening and exercise screening, but more likely to receive glucose testing, compared to private insurance patients. This finding suggests that health insurance status is a contributing factor in Medicaid at-risk CVD patients receiving some recommended CVD preventive services.
It is also important to underscore that Medicaid and private insurance patients at risk for CVD had low rates of five of the six recommended CVD preventive services. This finding suggests that at Medicaid and privately insured visits to PCPs in private practice, patients were not receiving a comprehensive set of clinical services for prevention of CVD. The low rates of CVD preventive services indicate a need for PCPs to increase clinical practices that reduce CVD among Medicaid and privately insured patients at risk for the disease. However, we cannot rule out the possibility that Medicaid and privately insured patients at risk for CVD were receiving recommended services at community health centers, hospital ambulatory care departments, or emergency departments.
A possible explanation for the low rates of recommended CVD preventive services for Medicaid patients at risk for CVD is that only three of the six recommended CVD preventive services (blood pressure screening, hemoglobin A1c test, and lipids/cholesterol screening) were included in the eCQM list used by CMS to assess whether eligible professionals are demonstrating meaningful use under the Medicaid EHR Incentive Program [16,23,24]. The development and implementation of eCQMs are beyond the scope of this paper. However, which eCQMs to select and report on under the Medicaid EHR Incentive Program is based on several factors, such as the list of endorsed and approved eCQMs by CMS. The exclusion of recommended clinical practice guidelines for CVD prevention from the eCQM list may be associated with low rates of recommended CVD preventive care and screening services for Medicaid patients. Further analysis to support this assumption is warranted.
Primary care physicians caring for Medicaid patients at risk for CVD were less likely to adopt fully functional CEHRT. The finding that PCPs treating Medicaid patients at risk for CVD were less likely than private insurance PCPs to adopt fully functional CEHRT is consistent with past analyses demonstrating that Medicaid providers had lower rates of EHR adoption compared to private insurance providers [25]. The variation in adoption of core EHR functionalities may exacerbate disparities in the provision of recommended preventive services for Medicaid patients at risk for CVD.
Notwithstanding blood pressure screening, across all CVD preventive care services, PCPs who adopted fully functional CEHRT were less likely to administer the recommended services to prevent CVD in at-risk adults. These results indicate a need for clinical providers and health IT professionals to collaborate on population health, patient engagement, care coordination, and quality improvement initiatives that prevent chronic diseases. For example, utilizing artificial intelligence, machine learning, and predictive analytics to electronically identify patients at-risk for CVD. Once identified and flagged within the EHR, when the patient presents for their primary care visits a "Best Practice Advisory" (BPA), also known as a best practice alert, could notify the clinician that they need to complete blood pressure screening, in addition to diet/nutrition counseling, exercise counseling, lipids/cholesterol screening, glucose level determination, and weight reduction counseling. Decision support tools, such as a BPA has been demonstrated across health care settings as an effective disease management tool within an EHR to alert providers that a specific patient population needs recommended services [26,27].
Findings were mixed with respect to the presence of core EHR functionalities for Medicaid versus private insurance providers. Medicaid and private insurance providers caring for patients at risk for CVD had similar adoption rates for all core EHR functionalities - except care coordination, in which Medicaid providers had lower rates of adoption. EHRs in primary care are an important tool for enhancing care coordination and facilitating provider collaboration [28]. Care coordination presents opportunities for improving chronic disease management in primary care [29]. As such, Medicaid patients at risk for CVD treated by PCPs without EHR care coordination decision support features may experience fragmented care that has the potential to adversely impact their experience, safety, and overall health. These findings must be considered in light of the findings demonstrating weak associations between core EHR care coordination functionalities and the provision of recommended CVD preventive services in the overall sample as well as subpopulations.
The likelihood of Medicaid-insured at-risk CVD patients receiving recommended CVD preventive services was not significantly higher for any specific core EHR functionality area, although we did find some significant results spread throughout the associations. More specifically, at Medicaid visits, having an EHR capable of generating a list of patients by diagnosis increased the probability that weight reduction counseling occurred at a PCV, implying that this feature facilitates an aspect of public and population health management.
This study has several limitations. First, these data are from 2014 and 2015 and may not reflect current levels of EHR adoption and the provision of recommended CVD preventive services. Another limitation is that the NAMCS is based on self-reports by physicians or staff members, which makes them vulnerable to recall bias. Additionally, self-reported data can lead to overestimates or underestimates of EHR adoption and the provision of CVD preventive services. Due to the nature of the sampling method inherent to the NAMCS survey, some degree of sampling bias cannot be ruled out, although efforts were taken to adjust for this bias. Given the cross-sectional design of the NAMCS survey data, we were not able to determine when the risk for CVD occurred. Lastly, this study did not take into consideration EHR vendor type, data architecture, electronic specifications, data elements, and end-user interface.
This analysis did not allow us to definitively determine whether EHRs integrated with CDS functions such as reminders, shared health information, population health management tools, and quality improvement features is associated with PCPs delivering recommended CVD preventive health services to adults with Medicaid at risk for CVD. Our findings also raise concerns about the rates of recommended CVD preventive services at PCVs for Medicaid patients at risk for CVD, which imply gaps in their care. Additional research is needed to better understand how the approved list of eCQMs impacts the provision of preventive care services recommended by notable health care institutions. Understanding the impact core EHR functionalities for public and population health management, care coordination, patient engagement, and quality improvement has on the provision of recommended preventive health services can help reduce the likelihood that at-risk low-income patients will be diagnosed with CVD. The results from this study can be used for the development of future research, policies, and clinical practice initiatives that incorporate EHRs and CDS functions targeting CVD prevention in underserved populations.