Epiphrenic diverticulum is a relatively rare clinical case. It is defined as an outpouching of the mucosal and submucosal layers through the muscular layer of esophagus in association with motility disorders. Most patients are asymptomatic and the other manifest with variable symptoms including dysphagia, regurgitation, halitosis, vomiting, heartburn and weight loss.
Herein we report a case of a 50-year-old female who presented to our hospital with complaint of dysphagia and weight loss. The clinical and radiological findings suggested left epiphrenic diverticulum about 3 cm in diameter.
As the best and most appropriate treatment, we performed laparoscopic transhiatal diverticulectomy, Heller esophageo cardiomyotomy and Dor anterior fundoplication. The patient was discharged home in the second day with some recommendations and she was well.
The main treatment of epiphrenic diverticula is diverticulectomy transhiatal via laparoscopy followed by Heller myotomy and antireflux procedure.
We advise surgeons to consider the operative approach because it is safe, effective and has less complications compared the other approaches.
Epiphrenic, Diverticulum, Laparoscopy, Esophageal, Case-report
Esophageal diverticulum is relatively a rare clinical case. According to the medical literature, it's prevalence is up to 3% due to radiological and endoscopic studies [1,2]. Anatomically, esophageal diverticula can be divided in to pharyngeal (Zenker), middle and distal (epiphrenic) [3].
Epiphrenic diverticulum is defined as an outpouching of the mucosal and submucosal esophageal layers throughout the muscular layer, so that it is considered as pulsion false diverticulum. It constitutes about 20% of all esophageal diverticula [4]. Although the etiology of this disease is undetermined, it is mostly associated with esophageal motility disorders like diffuse esophageal spasm, achalasia, nutcracker esophagus and nonspecific dysmotilities [5].
About 15 to 20% of the patients are symptomatic [6]. But those who are symptomatic, usually present with variable manifestations such as dysphagia, regurgitation, heartburn, halitosis and vomiting [7]. The definite diagnosis is put based on upper gastrointestinal contrast study and endoscopy. Other investigations sometimes may be required such as esophageal manometry and pH-monitoring [8].
This disease is sometimes managed conservatively. However, the effective therapy for the symptomatic case is surgery. The surgical treatment involves diverticulectomy and usually Heller cardiomyotomy which should be completed with antireflux procedure (Dor or Toupet) to prevent postoperative gastroesophageal reflux disease [9]. Laparoscopic transhiatal diverticulectomy, Heller myotomy and Dor fundoplication operation are successful procedures with low morbidity and less complications [10]. Here in, we report a case of epiphrenic esophageal diverticulum in a 50-year-old woman who was treated laparoscopically.
A 50-year-old woman presented to our hospital. She had been complaining of dysphagia and weight loss since two years ago. She had not significant past medical or surgical history. There was no history of drugs use and no family history of digestive diseases.
On physical examination, there was no specific findings, the abdomen was soft and not tender. Routine blood test and chest-X-Ray were within normal range. Contrast radiogram with barium swallow detected an overfill focus arising above the diaphragm on the left side approximately 3 cm in diameter, which may refer to epiphrenic diverticulum (Figure 1). We did not do esophago-gastrodudenoscopy because the device in our hospital was broken down and there was no another one in our city. Esophageal manometry revealed motility disorder and high lower esophageal sphincter pressure. These findings suggested diffuse esophageal spasm.
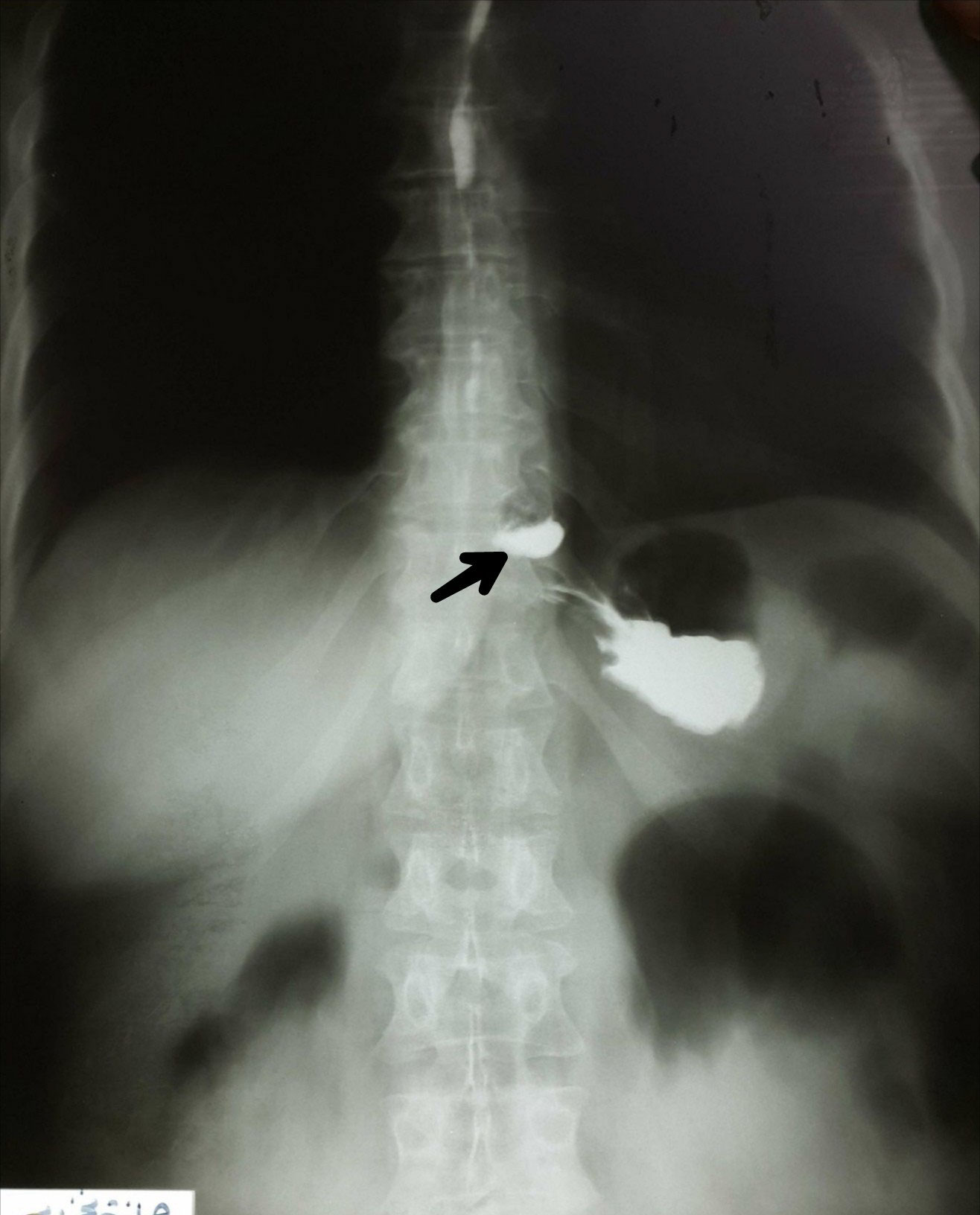 Figure 1: Contrast radiogram showed a diverticulum in the left side (arrow). View Figure 1
Figure 1: Contrast radiogram showed a diverticulum in the left side (arrow). View Figure 1
The patient then was admitted for surgical treatment after a good preparation. We selected the procedure of laparoscopic transhiatal diverticulectomy.
On the first postoperative day, a liquid diet was prescribed and the patient was discharged from hospital next day with some recommendations and soft diet for three weeks. On follow up for one year, she was in a good health state and gained weight normally. There was no complain of dysphagia or other symptoms.
The main surgical treatment for epiphrenic diverticulum is diverticulectomy which was traditionally done through thoracotomy (particularly the left side) or through laparotomy. This procedure is followed by myotomy on the other side of the esophagus and antireflux procedure [10]. As it is known that the pathophysiology of the epiphrenic diverticulum is still not clear, so this has mode the surgical approach controversial [11].
Laparoscopy is considered the choice of treatment for many esophageal diseases such as achalasia hiatal hernia and gastroesophageal reflux disease [12]. Furthermore, recently, laparoscopy has been the main approach because it enables good exposition of gastroesophageal transition, and eases myotomy and fundoplication [13].
In comparison with thoracotomy there are many advantages of laparoscopic approach, mainly: Higher safety, minimal postoperative pain, rapid recovery to life activities and shorter hospitalization [14,15].
In our case we performed laparoscopic transhiatal diverticulectomy, Heller cardiomyotomy using monopolar diathermy, and Dorl anterior fundoplication.
Patient was placed in 30° reverse Trendelenburg position while under general anesthesia. The surgeon stood between the patient's legs. Three ports were inserted in the abdominal cavity along the left costal arch 15 cm from each other, 1 port was placed in the epigastrium on the right side, and 1 port (10 mm in diameter) was inserted directly above the umbilicus (camera port). The abdominal and lower mediastinal segments of the esophagus were mobilized with a LigaSure device. Then the diverticulum was dissected and removed with stapler (Figure 2). The specimen was removed with an Endobag. After the diverticulectomy, a Heller esophagocardiomyotomy was performed on the opposite side of the proximal edge of the neck of the diverticulum in a segment 2 cm in length along the fundus, and then a Dor anterior fundoplication was performed (Figure 2).
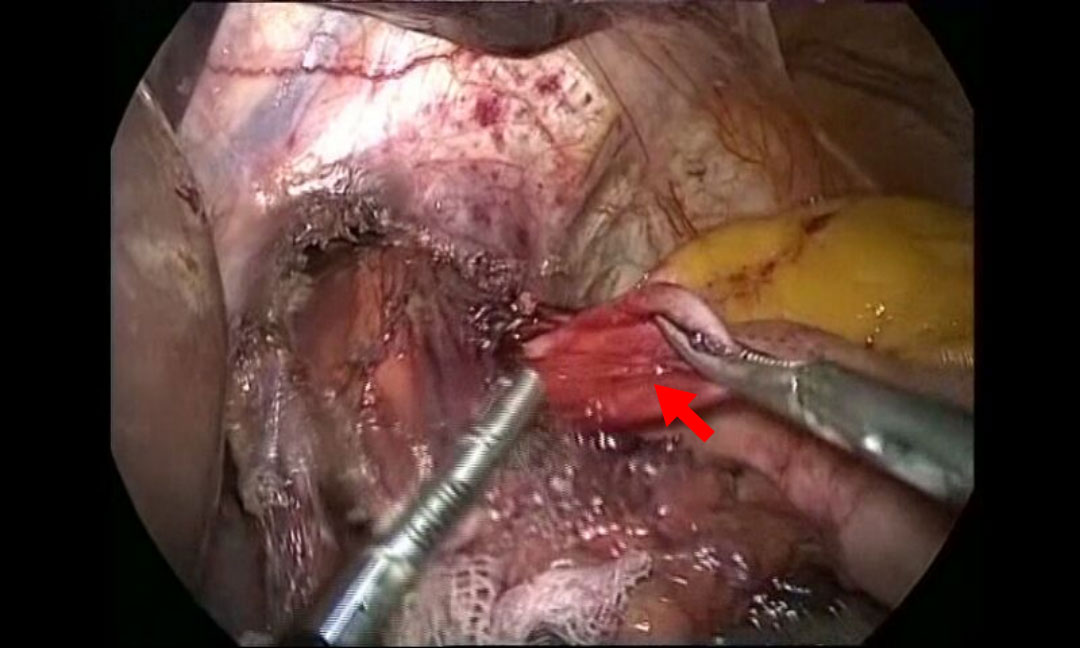 Figure 2: This image shows the Dor anterior fundoplication.
Figure 2: This image shows the Dor anterior fundoplication.
The red arrow indicates to the diverticulum. View Figure 2
Epiphrenic diverticulum is a relatively rare pathology. The most effective management is diverticulectomy with Heller myotomy and antireflux procedure. The operative approach should be appropriately selected to prevent any an unfavourable results or complications.
Laparoscopy is the preferable and safe approach. This method is efficient to improve symptoms and solve the problem but it should be performed by experienced surgeon.
Authors declare that there are no acknowledgements.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.