The aim of this article is to report an unusual case of inflammatory pseudotumor (IPT) that caused irreducibility of an inguinal hernia mimicking a tumour in the process.
A 64-year-old man presented with a 2 year history of reducible groin swelling which had progressively increased in size. The swelling had become irreducible 3 months prior to admission but apart from loss of weight, there were no other associated symptoms. He was anaemic (Hb 11 g/dL). At operation, a large, hard left inguinoscrotal hernia was encountered. This raised the suspicion of a tumour and therefore the testis and large mass were mobilised and resected along with an adherent segment of small bowel. He had end to end anastomosis of small bowel and modified Shouldice repair. He was well enough to self-discharge two days later and was well when seen two weeks postoperatively. The histological examination of the resected specimen confirmed an IPT and a normal testis.
The diagnosis and management of IPT remains elusive, however current evidence support histology as the mainstay of diagnosis and surgical resection as the first line of treatment.
Following surgical resection of IPT, it might be beneficial to follow up all cases to evaluate for recurrence and prompt management.
Inflammatory pseudotumor, Surgical resection, Benign tumour, Irreducible inguinal hernia
Inflammatory pseudotumor (IPT) is a benign lesion that affects virtually every anatomic site, mostly the lung but gastrointestinal tract rarely. IPT is a rare entity with few retrospective reviews in the paediatric population and small series report in the adult population [1]. IPT involving the gastrointestinal tract are uncommon. However, those that do occur involve in order of decreasing incidence, the stomach, small intestine, large intestestine and the oesophagus [2,3]. Its incidence is unclear and it is believed to affect both sexes equally. It is postulated that infection, trauma, surgical inflammation, immune-autoimmune condition and low-grade fibrosarcoma with inflammatory cells constitute important aetiological factors for IPT. A few have been found to be associated with IgG4-related sclerosing disease [2]. The aim of this article is to report an unusual case of IPT that caused irreducibility of an inguinal hernia mimicking a tumour in the process.
KM, a 64-year-old male presented with a 2-year history of left groin swelling which progressively increased to involve the scrotum. The swelling was initially reducible but had become irreducible three months prior to presentation with insignificant loss of weight but no associated pain, nausea, vomiting, abdominal distension or change in bowel movement. His past medical history included hypertension that was treated with Amlodipine 10 mg and Bendroflumethiazide 2.5 mg daily. On examination, he was neither pale nor jaundiced. His abdomen was soft with no organomegaly but had a left non tender irreducible inguinoscrotal swelling measuring approximately 14 × 8 × 6 cm. A full blood count revealed mild anaemia (haemoglobin 11.0 g/dl) but normal white cell and platelet counts.
At surgery under spinal anaesthesia, irreducibility of the hernia was found to be due to a hard mass within the hernia sac. Based on the suspicion of a potential tumour within the hernia sac or testis, a decision was made to deliver the sac and scrotal contents into the wound (Figure 1). As the testicle was normal in appearance, the sac was opened in order to inspect its contents. A bowel segment was firmly attached to a fleshy lesion measuring about 7 cm in diameter adjoining the testicle (Figure 2). The testicular appendage was divided and the small bowel adherent to the sac via fibrinoid adhesions was resected with end-to-end bowel anastomosis in two layers using 2 0 Vicryl and 4 0 PDS respectively. The testis along with the hernia sac was resected and the hernia defect closed using 2/0 Vicryl. A modified Shouldice repair was performed using 2/0 Nylon. He was well enough to self-discharge two days later and was well when seen two weeks postoperatively.
 Figure 1: Delivery of hernia sac with scrotal content into wound.
View Figure 1
Figure 1: Delivery of hernia sac with scrotal content into wound.
View Figure 1
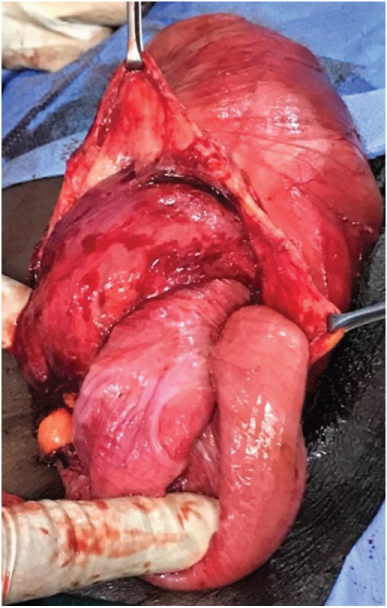 Figure 2: Opening of the hernia sac revealing the small bowel with the tumour.
View Figure 2
Figure 2: Opening of the hernia sac revealing the small bowel with the tumour.
View Figure 2
The resected specimen consisted of a fibrofatty tissue adjacent to but not infiltrating the wall of the bowel (Figure 3). It was a well demarcated fleshy lesion measuring 7 cm across with central cystic/myxoid degenerareas with intense chronic inflammatory changes. The hypocellular areas show stellate cells and wavy spindle cells admixed with foamy macrophages and cells showing signet ring configuration. The densely collagenized areas show intense chronic inflammation with numerous medium sized vessels. There were no mitotic figures and no evidence of malignancy. Changes were reported to be consistent with an IPT.
 Figure 3: Gross photograph of paratesticular lesion with a central cystic/myxoid degeneration.
View Figure 3
Figure 3: Gross photograph of paratesticular lesion with a central cystic/myxoid degeneration.
View Figure 3
The clinical presentation of IPT is mostly non-specific but depends on the site involved and relation to neighbouring structures. For example, IPT involving the pulmonary system presents with dyspnoea, pain, fever and cough while intraabdominal or retroperitoneal tumors present with abdominal pain, change in bowel movement, weight loss, symptoms of obstruction and as palpable masses. Furthermore, gastrointestinal IPTs may have features suggestive of malignancy, including ulceration, and infiltration of the wall. Our case presented with insignificant weight loss, mild anaemia and inability to reduce the groin swelling. Though adherent to the small bowel, the tumour did not infiltrate its wall. IPT presenting in an inguinal hernia as in this case is extremely rare as only one case has been reported in the literature - an 88-year-old male with IPT mimicking an incarcerated hernia [4,5]. Three histological characteristics have been described by recent studies; the first involves inflammatory cells and has myxoid stroma. The second has compact proliferation of spindle-shaped cells while the third has abundant collagen in a plate-like pattern [6]. Our case presented with a small bowel associated mass with histological features consistent with IPT though with mixed histological types.
IPT is similar to neoplastic processes clinically and radiologically hence making accurate diagnosis before surgery difficult. Our case presented with clinical findings consistent with irreducible inguinoscrotal hernia; therefore the decision before surgery with limited radiologic information was to do a mesh repair. As it turned out, imaging prior to surgery would have ensured a definite planned procedure with informed patient consent. Not surprisingly there are no typical radiological features of IPT. Ultrasonography reveals diverse pattern of echogenicity while contrast enhanced CT scans may reveal images compatible with the diagnosis [4]. On MRI, the appearance of these tumors is also variable; relative to skeletal muscle on T1-weighted images they are usually hypointense, and hyperintense on T2-weighted images, and heterogeneously enhanced after administration of contrast material [5]. CT scan and MRI were not available and would not have been affordable by the patient. This demonstrates one of the key challenges of surgery in low to middle income economies.
At surgery the hernia sac was found to have content suspicious of a tumour of testicular or bowel origin. This led to resection of small bowel with good margins and radical orchidectomy performed from an oncological point of view. A modified Shouldice repair of the hernia became the logical choice of technique as the wound was considered as contaminated by virtue of the bowel resection.
The first line of treatment of IPT is surgical resection which was done in our case with good margins. Options for non resectable IPTs include: use of steroids particularly for orbital IPTs; chemotherapy (such as cyclosporine, azathioprine, methotrexate, and cyclophosphamide); and COX II inhibitors [2,4,5,7]. Response to ancillary therapy is unpredictable. IPT has a tendency toward local aggressive behavior and recurrence. Rare cases of distant metastases and spontaneous remissions have also been described [5]. In a study of 53 cases of extrapulmonary tumors, 13 patients (25%) developed one or more recurrences at one to 24 months post resection. Nine of the patients that developed recurrence were found to have intraabdominal or retroperitoneal tumors with two undergoing histologic transformation into a higher grade sarcoma [7]. In another study of four cases involving the alimentary canal, one patient had two recurrences occurring at two (managed by surgical resection) and six (treated with oral anti-inflammatory drugs) months respectively [8]. These reported incidences of recurrence raises the need for medium to long term follow up with imaging after surgical resection of IPT.
This report adds another case of IPT to the literature and raises awareness about its occurrence. Surgical resection remains the first line of treatment of IPT and medium to long term follow up is essential to ensure prompt management of recurrence.
We thank Kafui P. Akakpo of the Department of Pathology, School of Medical Sciences, University of Cape Coast, Ghana for his help with reporting the slides.
EAA-Case report, literature search, discussion & write up
RH-Case report & discussion
MM-Ideas for discussion & critical review
JAA-Concept, write up & critical review.
None.