Hypoglycemia is one of the commonest metabolic problems in contemporary neonatal medicine. In the majority of healthy neonates, the frequently observed low blood glucose concentrations are not related to any significant problem and merely reflect normal processes of metabolic adaptation to extrauterine life. However, when low blood glucose levels are prolonged or recurrent, they may result in acute systemic effects and may result in neurologic sequelae.
To find out the incidence of hypoglycemia in exclusively breastfed high-risk newborns and to study associated risk factors like gender, gestational age, birth weight, time of onset of the development of hypoglycemia
This Descriptive Cross-sectional study of neonates enrolled 75 exclusively breastfed high-risk neonates (low birth weight, late preterms, small-for-gestation, large-for-gestation, infant of diabetic mother and macrosomic), who did not require admission to neonatal intensive care unit and were kept in postnatal wards with mother. Hypoglycemia was defined as blood glucose < 40 mg/dl. Blood glucose was monitored until 72 hours of life (at 2, 6, 12, 24, 48, 72 hrs of life).
The incidence of hypoglycemia in newborns with risk factors was 20% (15 of 75 neonates). All were asymptomatic. The incidence of hypoglycemia in SGA neonate was 37.5% (6/16), in LGA neonate was 18% (2/11), in Macrosomic neonates 20% (2/10), in LBW neonates 24% (9/38), in IDM was 14% (4/25) and in late preterm was 14% (2/12).In the present study, most of the neonates had hypoglycemia within 24 hours of life and none of the neonates were hypoglycemic after 48 hours of life.
We conclude that the incidence of asymptomatic hypoglycemia is fairly common in high-risk neonates. Strict monitoring and a close watch are therefore necessary to detect hypoglycemia and institute measures to prevent progression to symptomatic hypoglycemia and sequelae later on in life.
Hypoglycemia, Newborns, Incidence, Risk factors
Hypoglycemia is one of the commonest metabolic problems in contemporary neonatal medicine. In the majority of healthy neonates, the frequently observed low blood glucose concentrations are not related to any significant problem and merely reflect normal processes of metabolic adaptation to extrauterine life. However, when low blood glucose levels are prolonged or recurrent, they may result in acute systemic effects and neurologic sequelae [1]. The fetus in utero is entirely dependent on the mother for glucose. At the time of birth, the neonate must abruptly switch from having a continuous supply of glucose from the maternal blood in fetal life to maintaining its own supply of glucose during periods of fasting, and when feedings are interspersed intermittently [2]. Postnatal hypoglycemia in newborn infants remains an important clinical problem and prolonged periods of hypoglycemia may be associated with poor neurodevelopmental outcomes. Since prolonged periods of low plasma glucose are associated with increased risk of neurodevelopmental impairment, it is an important priority to prevent hypoglycemia in newborn infants [3]. Certain risk groups, including small for gestational age infants, preterm infants, and infants of diabetic mothers, are at high risk of hypoglycaemia [4]. Prevention, early diagnosis, and prompt treatment are important for high-risk infants who develop hypoglycemia, to minimize the severity and duration of hypoglycaemic episodes, which are associated with adverse outcomes [5]. This study aimed to find out the incidence of hypoglycemia in exclusively breastfed, high-risk newborns, and to study associated risk factors like gender, gestational age, birth weight, time of onset of the development of hypoglycemia.
This Cross-sectional, descriptive hospital-based study was carried out in the Postnatal ward of Nazareth hospital, Shillong from 15th January 2019 to 14th July 2019. A total of 75 newborns were included in the study. Ethical clearance for conducting the study was obtained from the institutional ethics committee. We included all high-risk healthy newborns who were exclusively breastfed after obtaining informed consent from the mother. The high-risk group was defined as small for gestational age (SGA) infants (birth weight less or equal to the 10th percentile for gestational age), large for gestational age (LGA) infants (birth weight more or equal to the 90th percentile for gestational age), low-birth-weight babies (birth weight less than 2500 g), macrosomic infants (birth weight more than 4000 g), infant of a diabetic mother (IDM) (maternal type 1 or type 2 diabetes mellitus or gestational diabetes mellitus), late preterm infant (LPI) (a premature infant born between 34-36 6/7 gestational week). The birth weight percentiles were adopted from the Lubchenco chart [6]. Newborns with a major congenital malformation in whom breastfeeding cannot be initiated, who required I.V. fluid, in whom exclusive breastfeeding cannot be continued or contraindicated were excluded. The detailed history of the enrolled babies was taken which included various maternal risk factors like GDM, PIH, twin pregnancy, etc, and neonatal risk factors like prematurity, LBW, SGA, etc.
Capillary blood samples were taken after warming the heels of the babies. Blood glucose concentration was determined by using the glucometer and test strips (SD CodeFree, SD BIOSENSOR). Capillary blood sugar was checked with a portable glucometer at 2 hours, 6 hours, 12 hours, 24 hours, 48 hours, and 72 hours of life and recorded. The babies were observed for signs and symptoms attributable to hypoglycemia. Hypoglycemia definition that was used in the study was blood glucose level below 40 mg/dl [7].
Following the detection of hypoglycemia, the neonates were managed as per institutional protocol. p-value < 0.05 was considered statistically significant.
During the study period, a total of 758 deliveries occurred. Overall 683 cases were excluded from the study: 502 newborns because of being non-high-risk; 5 newborns for having major congenital malformation; 173 newborns required I.V fluid; 3 newborns in whom exclusive breastfeeding could not be continued. The population demographics are depicted in Table 1 and Figure 1.
Table 1: Demographic data of the enrolled neonates and their mothers. View Table 1
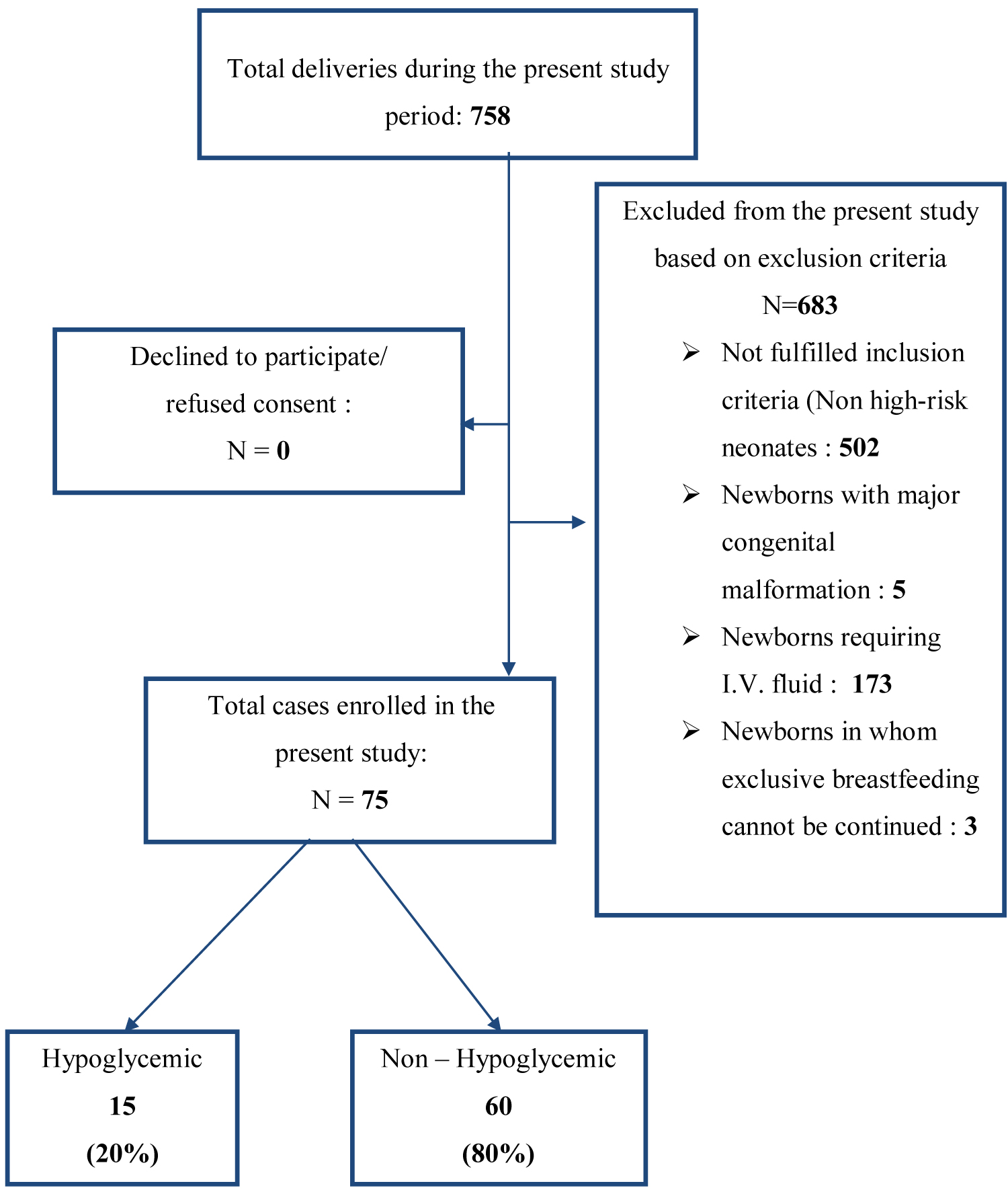 Figure 1: Flow diagram of the distribution of cases in the present study.
View Figure 1
Figure 1: Flow diagram of the distribution of cases in the present study.
View Figure 1
Of the 75 high-risk neonates that were enrolled in this study, 15 neonates developed hypoglycemia in the first 72 hours of life. So, the incidence of hypoglycemia in the high-risk newborns is found to be 20% in this study Table 2.
Table 2: Characteristics of high-risk neonates that were enrolled in the present study. View Table 2
In the present study, the neonates of multigravida mothers had a higher incidence of hypoglycemia than those of primigravida mothers. Hypoglycemia was found to be more in newborns whose mother’s age was > 30 years than in newborns whose mother’s age was < 30 years at the time of delivery and higher in neonates who were delivered through cesarean section than the vaginal route. These observations were found to be statistically significant after applying the tests of proportion Table 3.
Table 3: Characteristics of the hypoglycemic neonates (n = 15). View Table 3
In the present study, out of 38 LBW neonates 24% (9/38) neonates were hypoglycemic, which was found to be statistically significant. (Proportion test, p-value: 0.004). Out of 29 IDM 14% (4/29) neonates were hypoglycemic, which was found to be statistically significant. (Proportion test, p-value: 0.001). Out of 14 Late preterm neonates 14% (2/14) neonates were hypoglycemic, which was found to be statistically significant. (Proportion test, p-value: 0.02) Table 4.
Table 4: Distribution of hypoglycemia in the high-risk neonates in the present study (n = 75). View Table 4
In the present study, after analyzing the distribution of hypoglycemia and birth weight of the neonates, it was found that amongst the 38 low birth weight newborns, 23.7% (9/38) were hypoglycemic. (Proportion test, p: 0.004). Out of 27 normal birth weight neonates, 14.8% (4/27) were hypoglycemic. (Proportion test, p: 0.002). Whereas in Macrosomic newborns we did not see a statistically significant difference. (Proportion test, p: 0.1) Table 5.
Table 5: Distribution of hypoglycemia in the present study according to birth weight of the neonates (n = 75). View Table 5
On analysis of the hypoglycemic neonates and their gestational age, it was observed that among the 14 Late preterm newborns, 14.3% (2/14) were hypoglycemic, which was statistically significant. (Proportion test, p: 0.03). Out of 31 Early term neonates, 22.6% (7/31) were hypoglycemic, which was statistically significant. (Proportion test, p 0.007). Among the 28 Full-term newborns 17.9% (5/28) were hypoglycemic, which was statistically significant. (Proportion test, p 0.004) Table 6.
Table 6: Distribution of Hypoglycemia in the present study according to gestational age of neoantes (N = 75). View Table 6
Out of 15 newborns who developed hypoglycemia, all except one neonate developed hypoglycemia by 24 hrs of age: 26.7% (4/15) neonates had hypoglycemia at 2 hours of life, 40% (6/15) neonates had hypoglycemia at 6 hours of life, 20% (3/15) neonates had hypoglycemia at 12 hours of life, 6.7% (1/15) neonate had hypoglycemia at 24 hours of life, 6.7% (1/15) neonate had hypoglycemia in at 48 hours of life and none had hypoglycemia at 72 hours of life. This observation was found to be statistically significant (p-value: 0.01 - 1st 24 hours vs. > 24 hours of life). This further reinforces the fact that proper monitoring of blood glucose is highly essential for the first 24 hrs of life Figure 2.
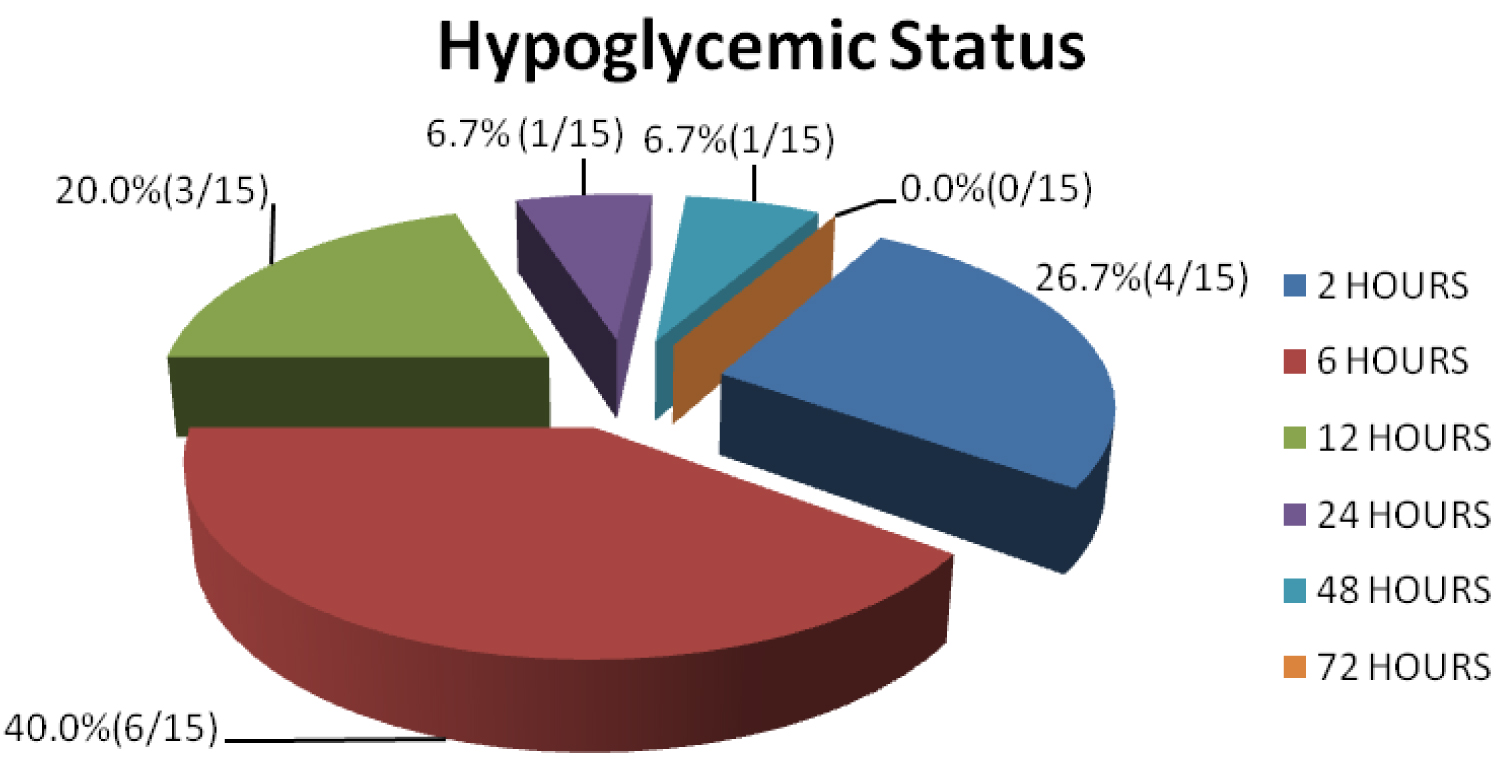 Figure 2: Detection of hypoglycemia in hours of life in newborns in the present study (n = 75).
View Figure 2
Figure 2: Detection of hypoglycemia in hours of life in newborns in the present study (n = 75).
View Figure 2
The authors of this study did not find any neonate with symptomatic hypoglycemia. None of the neonates required IV fluid therapy or NICU admission following the development of hypoglycemia. All were managed with frequent breastfeeding as per institutional policy.
In the present study, out of 75 newborns, 15 newborns were found to be hypoglycemic whereas 60 newborns did not have hypoglycemia. Hence the incidence of hypoglycemia in exclusively breastfed but high-risk neonates was 20% (Table 7).
Table 7: Various studies have shown a varying incidence of hypoglycemia. View Table 7
Various researchers have used different definitions of hypoglycemia, a variety of methods of detection of hypoglycemia and their studies have used different inclusion and exclusion criteria for their studies. Hence we see a wide variation in the incidence figures. Population characteristics may also have led to variation in the figures of incidence.
The relatively high incidence of hypoglycemia in this study amongst exclusively breastfed high-risk neonates born in a tertiary care hospital in Meghalaya could be attributed to certain population characteristics such as the high prevalence of multiparity and elderly gravidae. Meghalaya has a TFR 3 (NFHS 4 data) [18] which is the second-highest in the country and much higher than the national average of 2.2 [19]. This would have a cascading effect and lead to preterm births, late preterm births, and the birth of low birth weight neonates. This study also enrolled a relatively high number of Infants of diabetic mothers which is a reflection of the high prevalence of diabetes in the population.
In our study, the incidence of hypoglycemia in male neonates was found to be more than female neonates (27.3 vs. 14.3%). However, when the incidence of hypoglycemia was compared with each other it was concluded that hypoglycemia in exclusively breastfed high-risk newborns, did not have any sex predilection (p: 0.45). This observation was similar to the studies conducted by Saini A, et al. [10] from Haryana, India in the year 2018, and a study conducted by Jonas D, et al. [20] from Feldkirch, Austria the year 2014.
We found that the incidence of hypoglycemia in newborns was higher when maternal age was more than ≥ 30 years, but the results were different from the study conducted by Kumar TJ, et al. [9] in the year 2018, where they found that the incidence of hypoglycemia in infants born to mothers less than 30 years of age was 38%, while the incidence in infants born to ≥ 30 years was 18.9%. In our study, the enrolled subjects that were more than 30 years usually had multiparity and poor maternal health and had poor access to medical services.
In our study, the neonates of multigravida mothers had a higher incidence of hypoglycemia than primigravidae. Similar results were obtained by Sasidharan CK, et al. [21]. But result was different in the study which was conducted by Purnima Samayam, et al. [22] in the year 2015 where they found 23.07% of neonates born to primiparous mothers had hypoglycemia, against 5.4% neonates born to multiparous mothers. This finding can also be explained by the advanced age of the mothers (above 30 years) with poor maternal health and access to maternal health services in the multiparous mothers.
The infants who were delivered by cesarean section were found to be at higher risk for developing hypoglycemia in our study (p-value: 0.04). Potential mechanisms that might mediate this association include delayed lactogenesis, delayed skin-to-skin, and impaired thermoregulation
The present study has shown that the incidence of hypoglycemia was high in high-risk newborns. The blood glucose level of a newborn was affected by maternal factors like - parity of mother, maternal age, maternal morbidity, mode of delivery, and neonatal risk factors like gestational age and birth weight. There is no association between blood glucose level and sex of neonate, residence & religion of mother, and APGAR score.
We conclude that healthy high-risk newborns in the postnatal ward can be exclusively breastfed, but their blood glucose levels need to be monitored at least for the first 72 hours with the greatest emphasis on the first 24 hrs and asymptomatic hypoglycemia in newborns need to be detected and managed promptly.
Dr. Parth Patel was the principal investigator and the corresponding author; Dr. Palash Ranjan Gogoi and Dr. Santanu Deb were co-investigators; Dr. Prasenjit Paul, Dr. Pramod Paharia, Dr. Sabrina Yesmin, and Dr. Lima Sangla Jamir with all other authors prepared and reviewed the manuscript.
None.
None.