Choroidal metastases are the most frequent malignant intraocular tumor. In most cases, they arise after identification of the primary tumor and are associated with involvement of other organs. Less frequently, the ocular lesion may be the first presentation of a primary tumor or relapse of primary disseminated tumor.
Retrospective medical chart review including clinical and imaging investigations.
We present a case of choroidal metastasis as the first manifestation of recurrence of a breast tumor, diagnosed 4 years earlier. We analyze the clinical presentation, ancillary diagnostic tests and therapeutic indications.
The treatment of choroidal metastases aims at the recovery of visual function and the improvement of the quality of life, depending on the general state, number of lesions, location and laterality.
Choroidal metastases, Malignant intraocular tumor, Breast carcinoma
Uveal metastases are the most frequent malignant intraocular tumor, mostly localized in the posterior choroid (88-90%) [1-3]. This specific location seems to be related to the rich vascularization of the choroidal tissue which creates a microenvironment that predisposes to the development of tumor cells [2,4]. The primary tumors that most often metastasize to the choroid are breast (47%), lung (21%) and gastrointestinal (4%) [5].
The clinical presentation depends on the location, but the most frequent symptoms are blurred or decreased vision, floaters, photopsia and less frequently, pain [1,5,6]. Metastases originating from breast tumor are typically yellowish, plateau-shaped, associated with subretinal fluid and located at the posterior pole. Usually, they arise after diagnosis of the primary tumor and are associated with disseminated disease, involving other organs [6]. Ophthalmic multimodal imaging is decisive for diagnosis and follow-up [1]. Systemic workup is needed if there is no history of a primary tumor and an intraocular biopsy may be performed in suspect cases when other less invasive procedures are inconclusive [1,7].
The treatment depends on the extent of metastatic disease and may include chemotherapy (QT), hormonal therapy (HT), immune therapy (IT), intravitreal antiangiogenic treatment, photodynamic therapy and whole-eye external radiotherapy or plaque radiotherapy. The response to systemic and localized therapy is generally good, with lesion regression in 94% of cases and preservation of vision in 75% [1].
We report a case of a 51-year-old woman with a history of left breast adenocarcinoma for 4 years. The tumor was positive for human epidermal growth factor (HER2+) and the patient had been treated with tumorectomy, RT, QT and IT for 1 year (4 cycles of doxorubicin and cyclophosphamide followed by 12 cycles of paclitaxel and trastuzumab). She did well on routine follow-up, until she presented to the emergency department with a visual field defect in the right eye (RE), for 5 days. Her best corrected visual acuity (BCVA) was 6/10 in the RE and 10/10 in the left eye (LE). Fundoscopy revealed a yellowish elevated subretinal lesion near the inferior temporal arcade (Figure 1A). Optical coherence tomography (OCT) disclosed a hyporreflective choroidal lesion with undulating surface and compression of the choriocapillaris, associated with subretinal fluid (Figure 2A) and serous detachment of the fovea (Figure 3A). Based on clinical features and multimodal imaging, a presumed diagnosis of choroidal metastase (CM) was made.
 Figure 1: Fundus photography before (A) and after (B) treatment. A: Subretinal elevated yellowish lesion; B: Flat lesion with mottled appearance.
View Figure 1
Figure 1: Fundus photography before (A) and after (B) treatment. A: Subretinal elevated yellowish lesion; B: Flat lesion with mottled appearance.
View Figure 1
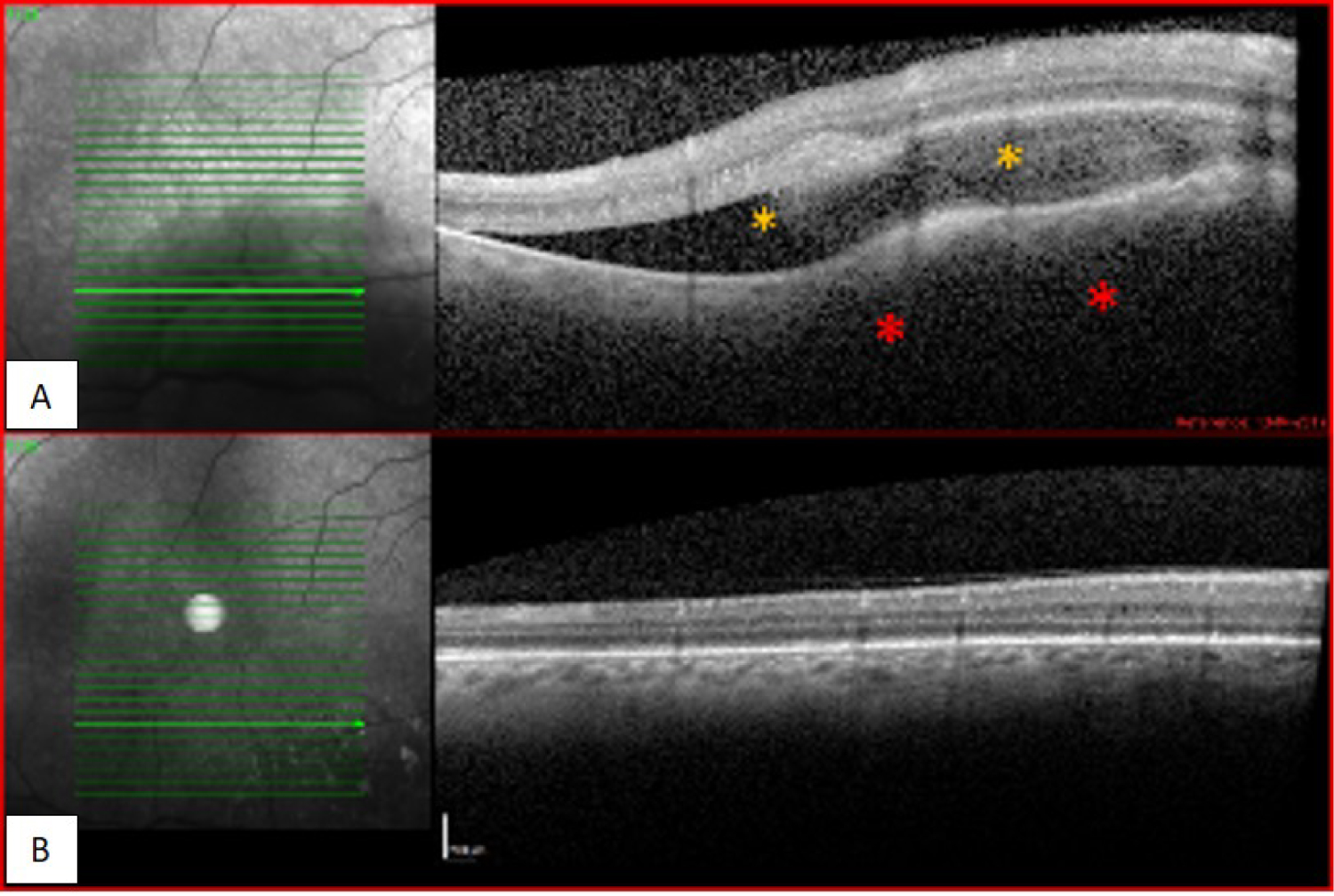 Figure 2: OCT at the level of the lesion, before (A) and after (B) starting treatment. A: Choroidal lesion with undulating surface (*) and compression of the choriocapillaris, associated with sero-fibrinoid subretinal fluid (*); B: Flattening of the choroid, without subretinal fluid.
View Figure 2
Figure 2: OCT at the level of the lesion, before (A) and after (B) starting treatment. A: Choroidal lesion with undulating surface (*) and compression of the choriocapillaris, associated with sero-fibrinoid subretinal fluid (*); B: Flattening of the choroid, without subretinal fluid.
View Figure 2
 Figure 3: OCT at the level of the fovea, before (A) and after (B) starting treatment. A: Serous detachment of the fovea (*) with normal neural retinal layer structure; B: Fovea without change.
View Figure 3
Figure 3: OCT at the level of the fovea, before (A) and after (B) starting treatment. A: Serous detachment of the fovea (*) with normal neural retinal layer structure; B: Fovea without change.
View Figure 3
Other secondary lesions were investigated by imaging – thoracic and abdominal computed tomography (CT) and brain magnetic resonance imaging (MRI), which revealed multiple pulmonary and brain metastases.
The patient started treatment with paclitaxel and trastuzumab followed, 3 weeks later, by cranial and ocular external beam radiation therapy (EBRT). After the first cycle of QT, the patient reported visual improvement and after 3 months of treatment, BCVA had recovered to 10/10. Fundoscopy demonstrated complete resolution of the choroidal lesion (Figure 1B), confirmed on OCT (Figure 2B and Figure 3B).
The patient´s systemic disease responded to the treatment regimen with total resolution of the metastatic brain lesions and a reduction in the number and size of the lung metastases.
Breast tumor is the most common malignant tumor in women and is associated with high morbidity and mortality. Despite the latest advances in diagnosis and therapy, in about 1/3 of cases, systemic dissemination will occur, including ocular metastases [4]. Our patient presented with a history of HER2+ breast tumor, for 4 years with no apparent progression of the disease, until the onset of ocular symptoms.
Clinical features and imaging tests were consistent with the diagnosis of CM. The patient had RE visual dysfunction and an amelanotic subretinal mass in the posterior pole, which is the main location of CM [1,5,7]. Diagnosis is aided by several ancillary test, particularly OCT tomographic features of hyporeflective choroidal lesions with lumpy-bumpy surface, compression of the choriocapillaris, subretinal fluid and intact retina internal layers [8].
Although in most cases CM arise after identification of the primary tumor and are associated with involvement of other organs, especially lung, brain and bone, they may also be the first presentation of the primary (4-46%) or disseminated tumor (12-31%) [9,10]. In our case the visual field defect was the presenting symptom which triggered the ocular and systemic evaluation and the recognition of disease progression.
The treatment is multidisciplinary and aims at the control of the primary tumor and metastases, with the fewest possible side effects. The choice between localized and/or systemic therapy depends on the general status of the patient, number of lesions, location and laterality [1,2]. Tamoxifen or aromatase inhibitors may be effective in tumors expressing estrogen or progesterone receptors and trastuzumab may be used in tumors expressing HER2 receptors [11]. These treatments, in association with QT, can lead to complete regression of the ocular lesions, in 1-4 months [12,13], avoiding the adverse effects of radiotherapy, particularly keratopathy, cataract, retinopathy and optic neuropathy [11].
Our patient was HER2+ and had disseminated disease; therefore she started combined systemic treatment (paclitaxel and trastuzumab) with visual improvement at the end of the first cycle. However, due to the presence of brain metastases, the patient was proposed for fractioned cranial and ocular ERBT. This combined treatment resulted in marked improvement of her general status with complete resolution of brain and choroidal lesions and partial resolution of lung metastases. The recovery of visual function was objectively confirmed on OCT scans which demonstrated normal choroidal structure with resolution of the subretinal fluid.
This case highlights the early and prompt diagnosis of ocular metastases and the efficacy of combined systemic and local treatment in the management of disseminated disease (choroid, brain and lung). The ophthalmologist may be the first physician to detect disseminating disease and the presence of choroidal metastasis should always lead to the investigation of lesions in other target organs.
The current therapeutic options allow for good results with high regression rates of ocular metastases. However, recurrences do occur, as well as metastases in the fellow eye. Thus, ophthalmologic examination should be continued periodically. OCT is a non-invasive high-resolution structural examination that enables the diagnosis and follow-up of CM.