Left ventricular pseudo-aneurysm (LVPA) is an infrequent complication of MI, occurring of an average of 3-14 days following acute myocardial infarction [1]. Most common site is posterior region; however, it may bulge in the apical, lateral and inferior cardiac wall [1]. LVPA contains neither endocardium nor myocardium, whereas the pericardial adhesions and thrombus seal off myocardial rupture. This time-bomb is prone to rupture, thus urgent surgery is indicated once LVPA is diagnosed [2].
Although surgery is the key-management of LVPA, however, high risk LVPA surgeries including: Reduced LVEF, concomitant mitral regurgitation requiring mitral valve replacement [3] and other systemic co-morbidities, highlighted the role of medical management toward these group of patients.
Current literature presented numerous cases of conservative management of LVPA [4,5], with reasonable outcomes of a median of 3.8 years [6]. With a 50% mortality on medical therapy [7].
Left ventricular pseudo-aneurysm, Trans-thoracic echo, Coronary bypass graft, Coronary angiography, Diabetes mellitus, Hypertension
LVPA: Left Ventricular Pseudo-Aneurysm; TTE: Trans-Thoracic Echo; CABG: Coronary Bypass Graft; CAG: Coronary Angiography; DM: Diabetes Mellitus; HTN: Hypertension
A 65-years-old gentle-man, heavily smoker (2 pocket per day).
Unknown history of HTN or DM, history of CVA 10 years ago (currently no motor abnormalities, presumably TIA), history of CAG 9 years ago for unknown complaint with normal coronary vessels flow (History of CVD).
Aspirin 81 mg PO once daily, Bisoprolol 5 mg PO once daily, inhaler Ventolin when needed.
The patient was transferred from abroad hospital due to its medical costs, after performing a diagnostic CAG without PCI. However, the gentle-man did not have documents from his previous hospitalization but the videos of the CAG. Also, the patient has an undefined type of ACS due to the lack of information.
The patient was asymptomatic when he consults the cardiovascular department in Tishreen University Hospital.
Chest discomfort, orthopnea, palpitation, peripheral edema, jugular vein pressure, hepatojugular reflux: Within normal values.
NYHA II Dyspnea evolved over the last year.
Vital signs on admission:
BP: 120\80
Spo2: 95%
Pulse: 100 bpm
Respiratory rate: 17
1) Admission ECG: Ventricular tachycardia originating from the left ventricle (130 BPM) (Figure 1).
 Figure 1: Admission ECG.
View Figure 1
Figure 1: Admission ECG.
View Figure 1
2) Department ECG (after administration of 300 mg I.V Amiodarone): NSR, 79 BPM, QS pattern on V1\V2, PRWP, LA enlargement pattern (Figure 2).
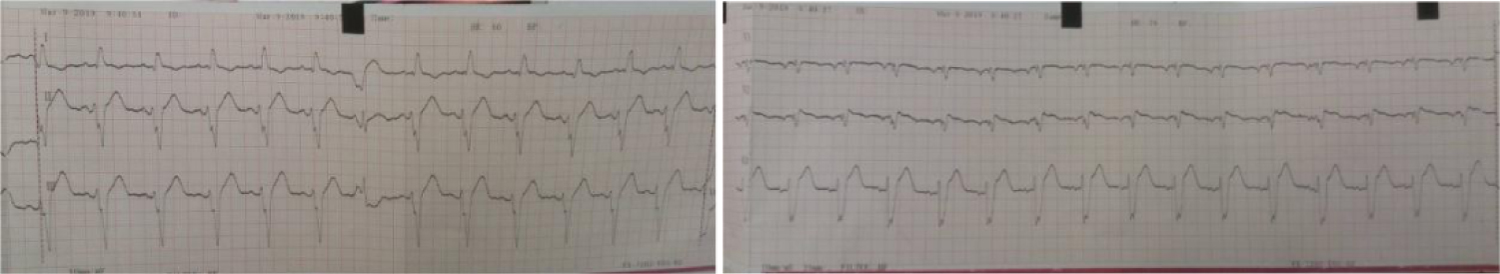 Figure 2: Department ECG.
View Figure 2
Figure 2: Department ECG.
View Figure 2
Wide mediastinum, bulging at the apex (Figure 3).
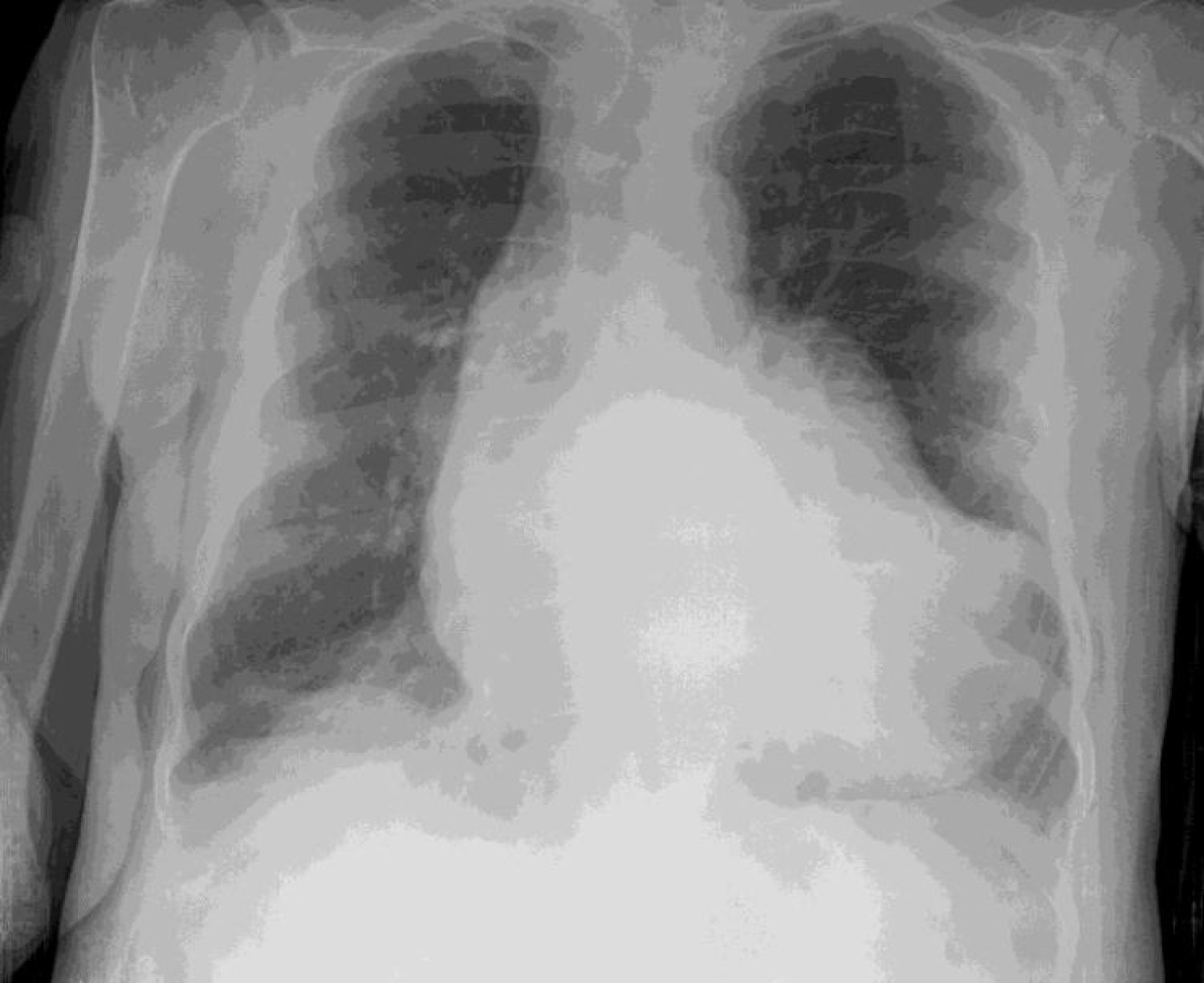 Figure 3: Chest X- ray (CXR).
View Figure 3
Figure 3: Chest X- ray (CXR).
View Figure 3
1) Dilated LV, poor LV systolic function and LV remodeling (Figure 4A).
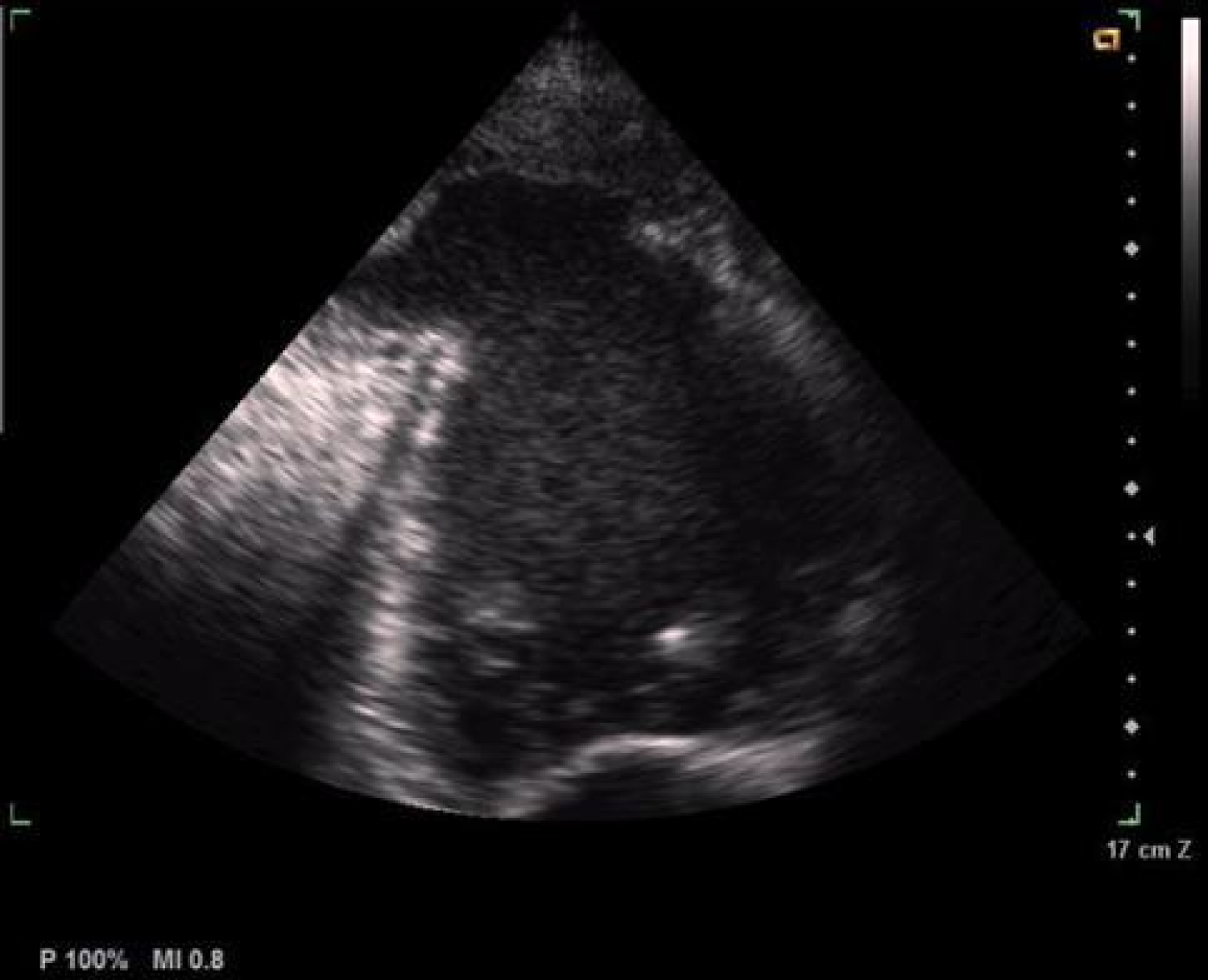 Figure 4A: Dilated LV, poor LV systolic function and LV remodeling.
View Figure 4
Figure 4A: Dilated LV, poor LV systolic function and LV remodeling.
View Figure 4
2) Pseudo-aneurysm at the apex of the LV with abrupt transition from normal myocardium to the aneurysm, a ratio of the neck diameter to the maximum diameter < 50%, a narrow neck at the site of rupture and partial filling of the aneurysm with thrombus (Figure 4B).
3) SPE: Spontaneous Echo Contrast in the LV (Figure 4C).
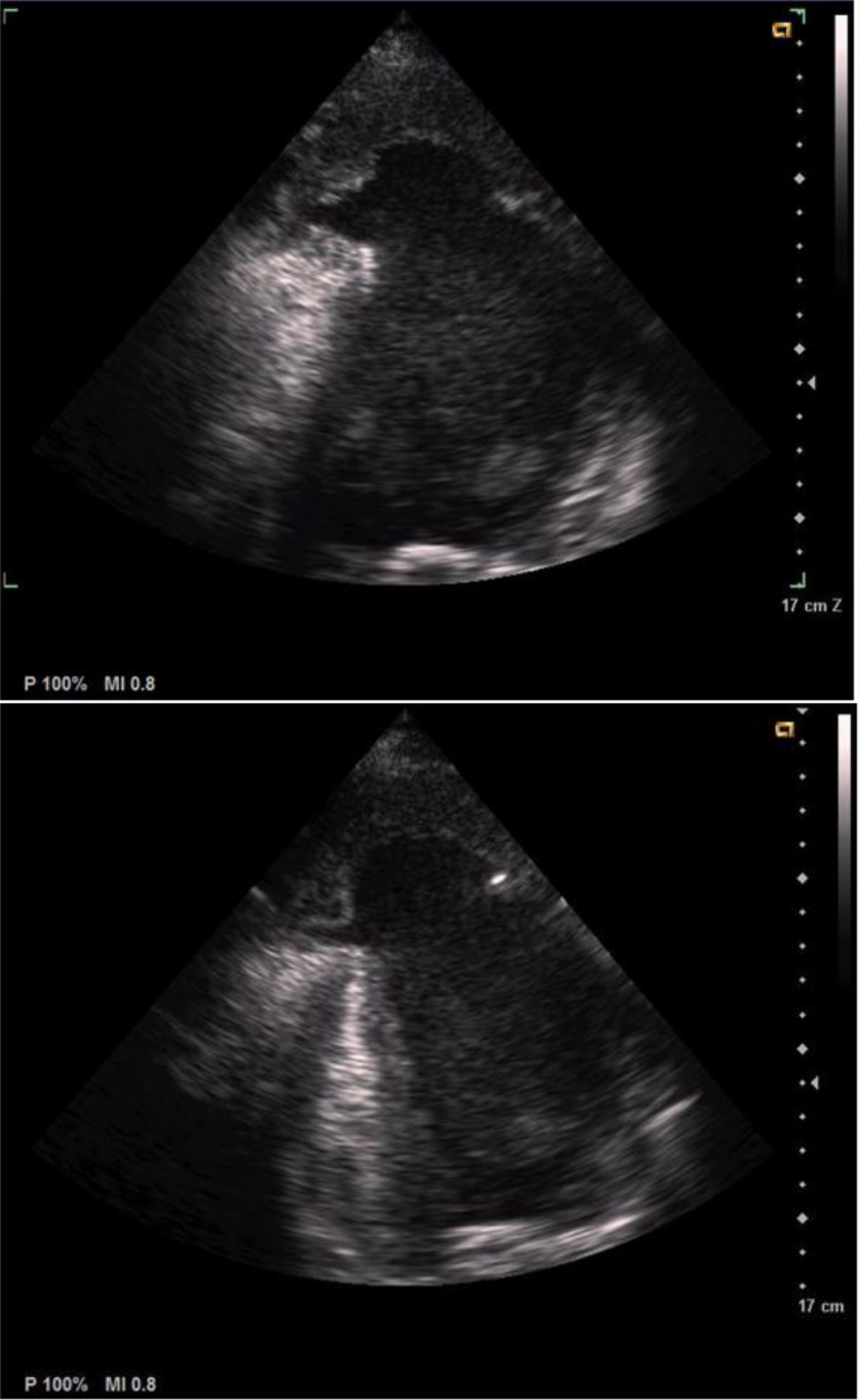 Figure 4: B) Pseudo-aneurysm at the apex of the LV; C) Spontaneous echo contrast in the LV.
View Figure 4B-C
Figure 4: B) Pseudo-aneurysm at the apex of the LV; C) Spontaneous echo contrast in the LV.
View Figure 4B-C
Patient refused any medical intervention (surgery) after the recognition of the surgical risk of a combined CABG/LVPA Repair.
Patient was discharged after one week on a GDMT for Chronic Heart Failure, with a monthly follow-up in the cardiac ward. Unfortunately, patient died within one month of admission.
Surgical repair of post infarct left ventricular pseudo-aneurysm was associated with an acceptable surgical mortality rate [8]. However, conservative management in selected patients with increased surgical risk seems reasonable [9]. But until large studies confirm the favorable outcomes of medical management, the preferred approach would remain surgical management.