An abnormal ankle-brachial index (ABI) is associated with higher risk for future cardio-vascular (CV) events; however, it is unknown whether this association is true in patients with associated diabetes mellitus (DM).
The objective of this study was to determine frequency of coronary artery disease in terms of number of vessels involved using angiography in diabetic patients with abnormal ankle brachial index.
This Cross Sectional Study was done at Department of Adult Cardiology, CPE institute of Cardiology Multan. ABI was measured using the standard method. After measuring the ABI, angiography was done on patients with abnormal ABI and pattern of Coronary Artery Disease (CAD) was recoded noting the number of vessels involved.
A total of 115 patients were included in the study. The mean age of patients was 62.40 years with standard deviation of 2.78 years. Majority of the patients in the study were male (68.7%). Mean ABI was of study participants was 1.2 with standard deviation of 0.58 while mean duration of disease was 3.2 years with standard deviation of 0.7 years. 97 of the study participants were hypertensive and 18 were smokers. A total of 28 patients (24.3%) did not have CAD as per angiography while the rest had 1 vessel disease (33.4%), 2 vessel disease (29.5%), and 3 vessel disease (20.9%). Stratification of patients by age, gender, duration of disease, hypertension and low/high ABI showed p value > 0.05 in all cases showing statistically insignificant difference between various subgroups.
It is concluded that there is high frequency of CAD in diabetic patients with abnormal ABI.
Coronary artery disease, Ankle brachial index, Peripheral arterial disease
Ankle-brachial index (ABI) has been suggested as a useful predictor of generalized atherosclerosis; individuals with a low ABI have an increased risk of death from cardiovascular disease (CVD) in epidemiological studies 1. ABI is an inexpensive and reliable method for detection of peripheral artery disease (PAD), and it has also been proposed as a marker of subclinical atherosclerosis and cardiovascular prognosis [1,2]. PAD caused by atherosclerotic occlusion in the arteries of the legs, is an important manifestation of systemic atherosclerosis and is defined as an ankle-brachial index ABI (≤ 0.90). Diabetes is a powerful risk factor for PAD, and the measurement of ABI is used to detect PAD in diabetic patients 3. However, in diabetic patients, it is not infrequent to find very stiff and even incompressible ankle arteries, leading to a high ABI (> 1.40). This situation is due to the presence of medial calcinosis (MC), a specific disease distinct from atherosclerosis, corresponding to the calcification of the medial layer, without protrusion into the arterial lumen [3]. Thus, it is important to study the pattern of CAD in diabetic patients with abnormal ABI as the results can be confounded by MC.
This study is prompted to examine the relationship of ABI with vessel involvement and degree of stenosis on angiography in Pakistani diabetic patients with abnormal ABI. The present study will help in clarifying the exact burden of the CAD in diabetic patients with abnormal ABI. This study, by determining the burden of CAD in diabetic patients with abnormal ABI, will be helpful selecting and referring patients for timely angiography thus decreasing mortality in this group of patients with high burden of silent CAD. It is also important to study this because it causes significant disease and financial burden. The study will be a valuable contribution as diabetes is a major public health problem in Pakistan.
The objective of this study was to determine frequency of coronary artery disease in terms of number of vessels involved using angiography in diabetic patients with abnormal ankle brachial index.
ABI was obtained using a standard protocol by placing patients in a supine position for at least 5 minutes. Systolic blood pressure of the brachial artery of both arms and the posterior tibial artery of both ankles was measured using a doppler probe. The highest blood pressure in the arms was be used to calculate ABI. The ratio of ankle to arm systolic blood pressure was calculated for each leg and the lowest ratio was recorded as the ABI for the patient. The ABI results were categorized among one of the following groups: low ABI (≤ 0.90), normal ABI (0.91-1.39), and high ABI (≥ 1.40). ABI ≤ 0.90 and ≥ 1.40 was taken as abnormal.
Patients were classified as having DM if they are receiving treatment with oral hypoglycemic agents or insulin for more than a year.
It was assessed on angiography in terms of number of vessels involved viz., 1,2,3.
Cross Sectional Study.
The study was conducted in Department of Adult Cardiology, CPE institute of Cardiology Multan.
6 months after approval of synopsis.
01.01.2016 to 30.06.2016.
Sample size was calculated to be 115 with 95% confidence interval, 10% margin of error and 11.8% expected frequency of CAD2 (one vessel disease) in diabetic patients abnormal ABI using WHO sample size calculator.
Non probability consecutive sampling.
• Diabetic patients with disease duration more than one year as per operational definition
• Both Genders
• Aged 50-70 years
• ABIs of patient in abnormal range low ≤ 0.9; high > 1.4.
• Patients with unstable cardiopulmonary, neurological, or psychiatric disease based on history and/or previous medical record
• Patients having vascular surgery of lower limbs as determined from medical record and history/examination.
• Patients not willing to participate in the study.
115 patients with diabetes mellitus who fulfill the inclusion and exclusion criteria were included in the study after taking Informed consent. ABI was measured using the standard method described previously. ABI ≤ 0.90 and ≥ 1.40 was taken as abnormal. After measuring the ABI, angiography was done on patients with abnormal ABI and pattern of CAD was recoded noting the number of vessels involved and degree of stenosis. Biodata was be entered in a predesigned structured proforma.
Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 16. Qualitative data like gender, presence of CAD, low/high ABI, hypertension, smoking history were presented as frequencies and percentages. Quantitative data i.e., age, ABI, duration of disease, number of vessel involved, were presented as means and standard deviations. Effect modifiers like age, gender, duration of disease, hypertension, low/high ABI, were dealt with through stratification. Post stratification chi square test was applied with p value < 0.05 was taken statistically significant.
A total of 115 patients were included in the study. The mean age of patients was 62.40 years with standard deviation of 2.78 years with most of the patients in the age range 61-70 years. Age distribution of the patients is given in Figure 1. Majority of the patients in the study were male (68.7%). Gender distribution is outlined in Figure 2. Mean ABI of study participants was 1.2 with standard deviation of 0.58. Classification of ABI is given in Figure 3. Mean duration of disease was 3.2 years with standard deviation of 0.7 years, outlines in Figure 4, Table 1. The 97 of the study participants were hypertensive and 18 were smokers, given in Figure 5, Figure 6 respectively.
 Figure 1: Age distribution, n = 115, Mean ± SD: 62.40 ± 2.78 years.
View Figure 1
Figure 1: Age distribution, n = 115, Mean ± SD: 62.40 ± 2.78 years.
View Figure 1
 Figure 2: Gender distribution, n = 115.
View Figure 2
Figure 2: Gender distribution, n = 115.
View Figure 2
 Figure 3: ABI distribution, n = 115, Mean ± SD: 1.2 ± 0.58.
View Figure 3
Figure 3: ABI distribution, n = 115, Mean ± SD: 1.2 ± 0.58.
View Figure 3
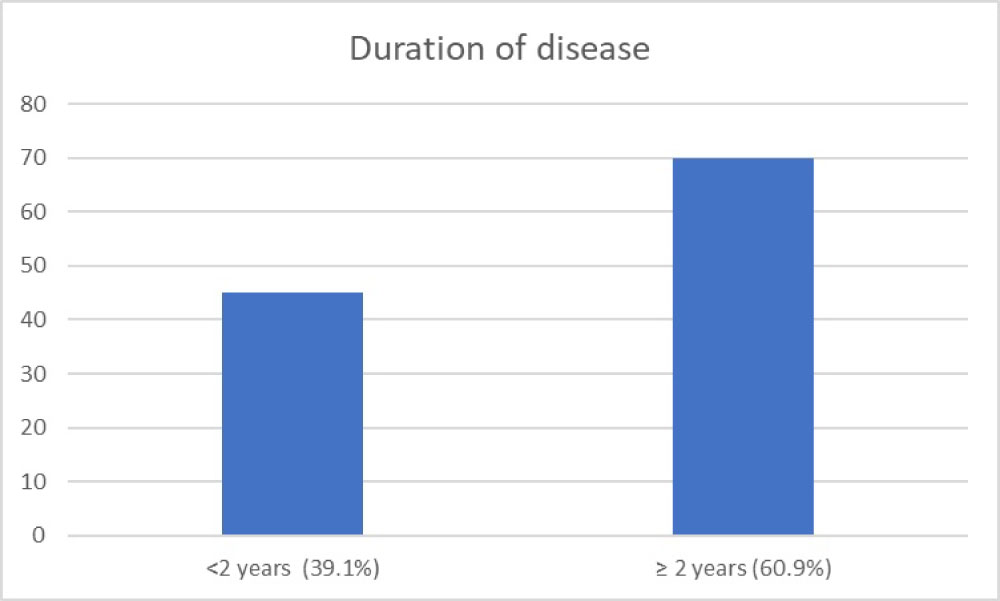 Figure 4: Duration of disease, n = 115, Mean ± SD: 3.2 ± 0.7 years.
View Figure 4
Figure 4: Duration of disease, n = 115, Mean ± SD: 3.2 ± 0.7 years.
View Figure 4
 Figure 5: Frequency of hypertension, n = 115.
View Figure 5
Figure 5: Frequency of hypertension, n = 115.
View Figure 5
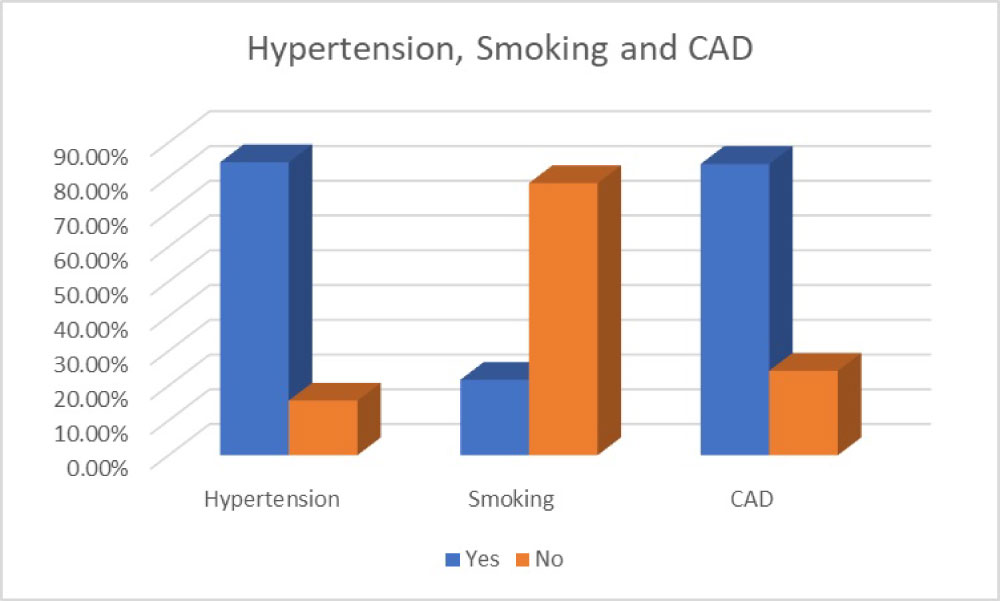 Figure 6: Frequency of hypertension, n = 115.
View Figure 6
Figure 6: Frequency of hypertension, n = 115.
View Figure 6
Table 1: Combination of Figure 1, Figure 2, Figure 3 and Figure 4. View Table 1
A total of 28 patients (24.3%) did not have CAD as per angiography while the rest had 1 vessel disease (33.4%), 2 vessel disease (29.5%), and 3 vessel disease (20.9%) given in Figure 7. Stratification of patients by age, gender, and duration of disease, hypertension and low/high ABI is given in Figure 8, Figure 9, Figure 10, Figure 11, Figure 12 and Figure 13 respectively. P value was > 0.05 in all cases showing statistically insignificant difference between various subgroups.
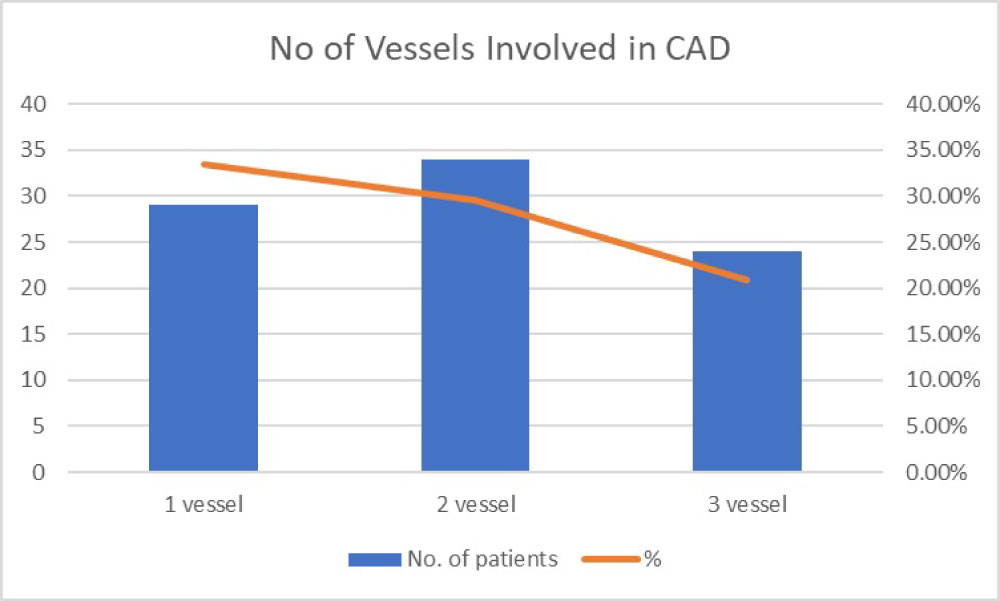 Figure 7: No. of vessel involved in CAD, mean number of vessels involved 1.76 ± 0.32.
View Figure 7
Figure 7: No. of vessel involved in CAD, mean number of vessels involved 1.76 ± 0.32.
View Figure 7
 Figure 8: Stratification by Age (n = 115).
Figure 8: Stratification by Age (n = 115).
Chi Square Test, Value: 0.258, Df: 3, P value: 0.878.
View Figure 8
 Figure 9: No. of vessels involved, stratification by age.
View Figure 9
Figure 9: No. of vessels involved, stratification by age.
View Figure 9
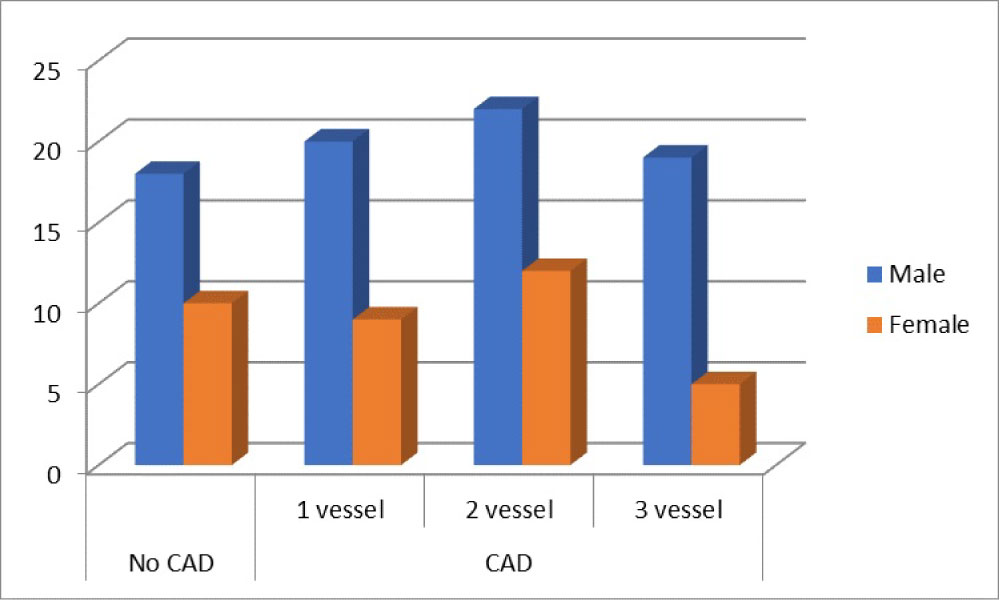 Figure 10: Stratification by gender.
Figure 10: Stratification by gender.
Chi Square Test, Value: 0.019, Df: 3, P value: 0.891.
View Figure 10
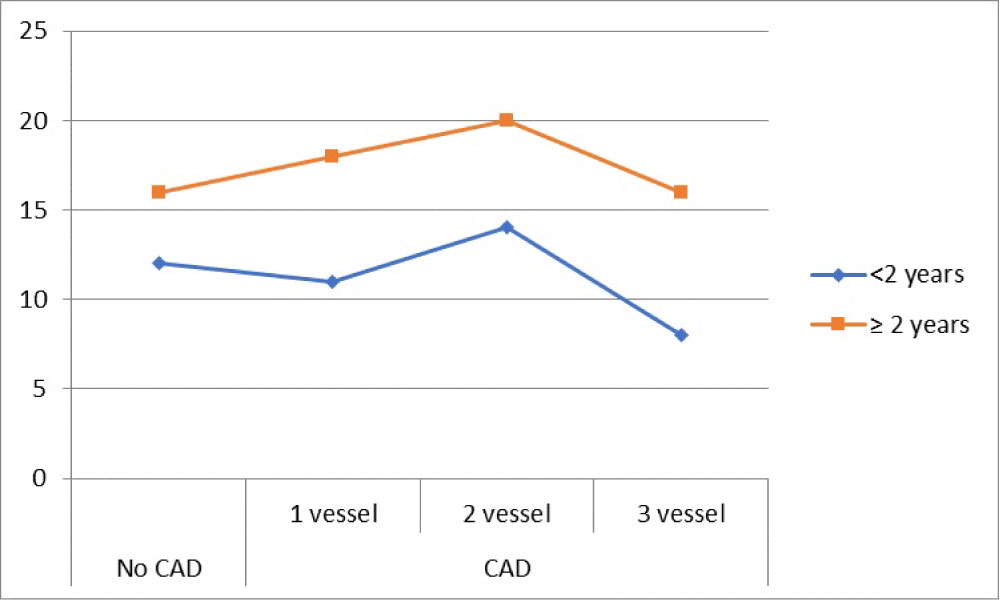 Figure 11: Stratification by duration of diseases.
Figure 11: Stratification by duration of diseases.
Chi Square Test, Value: 0.085, Df: 3, P value: 0.770.
View Figure 11
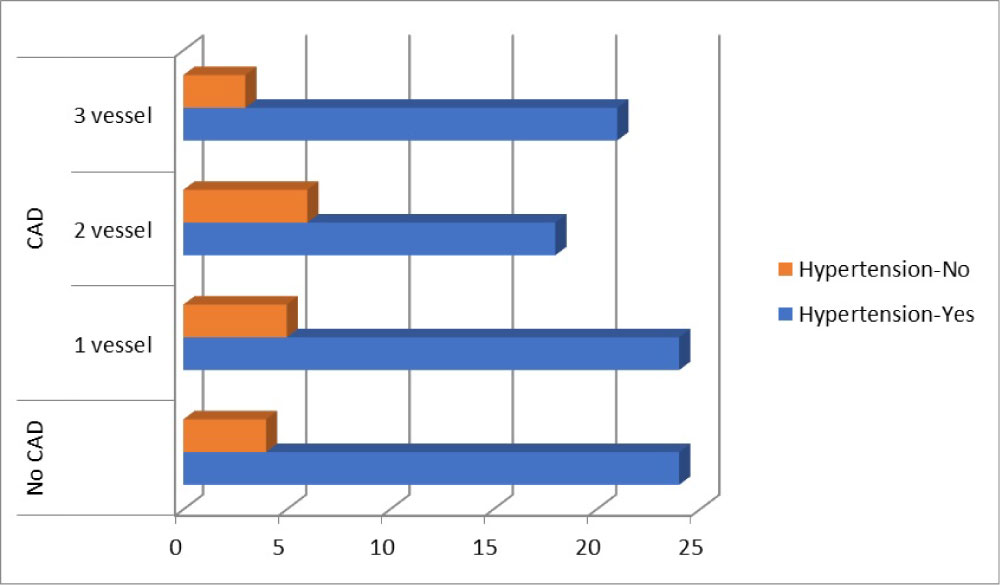 Figure 12: Stratification by hypertension, n = 115, P = 0.804.
View Figure 12
Figure 12: Stratification by hypertension, n = 115, P = 0.804.
View Figure 12
 Figure 13: Stratification by low/high ABI, n = 115, P = 0.770.
View Figure 13
Figure 13: Stratification by low/high ABI, n = 115, P = 0.770.
View Figure 13
The findings of this study are in agreement with some previous studies and reinforce the importance of screening for ABI and CAD in diabetic patients.
The findings of our study underscore the facts that there is significant overlap between CAD and PAD and that the identification of PAD in patients with stable CAD may provide important prognostic information in addition to the presence of DM, an independent and important risk factor for death and myocardial infarction.
The overlap between PAD and CAD has been established on the basis of various population-based studies [3-5]. Although the prevalence and outcomes of associated CAD in patients with PAD are well defined, there are limited data on the prevalence and prognostic significance of establishing the diagnosis of PAD in patients with stable CAD. Studies that have investigated the predictive value of ABI in a patient cohort with CAD are scarce. Dieter, et al. reported a 40% prevalence of PAD in hospitalized patients with CAD and the feasibility of performing an ABI in that setting [6]. Grenon, et al. reported a 70% increased risk of subsequent CV events (adjusted HR 1.7, 95% CI 1.0 to 2.9, p ¼ 0.04) and an 80% increased risk of death (adjusted HR 1.8, 95% CI 1.2 to 2.7, p ¼ 0.006) after adjusting for traditional risk factors [7]. Evidence from the Strong Heart Study identified the association between an abnormal ABI and mortality, highlighting a U-shaped relation between this noninvasive measure of PAD and mortality risk [8]. It also identified the cutoff values of abnormal ABI (< 0.9 and > 1.4), adopted by the American College of Cardiology (ACC) and American Heart Association (AHA) PAD guidelines and also used in our analysis [9]. Evidence from the Coronary Artery Surgery Study indicated that in patients with CAD, presence of PAD had a 25% greater likelihood of mortality than patients without (multivariate chi-square 25.83, HR 1.25, 95% CI 1.15 to 1.36, p < 0.001) [10].
The increased vulnerability to CV events in patients with CAD with an abnormal ABI can be partially explained by shared CV risk factors and excess inflammation indicated by significantly higher serum levels of inflammatory bio-markers in this patient population [11,12]. The higher repeat coronary events and revascularization rate in patients with CAD and PAD, observed in our study, can be potentially attributed to the significantly greater constrictive remodeling and plaque progression of atherosclerotic coronary arteries in patients with PAD.
In a recent study Mostaza, et al. reported that in patients with CV disease, ABI is a good predictor of the risk of recurrent CV events and death, however, only in subjects without DM [13]. The investigators argued that the presence of DM in patients with already established CV disease in itself confers such a high risk that an abnormal ABI does not add any prognostic value. As the CV outcomes in patients with CAD are strongly influenced by secondary prevention strategies, the findings from our study conducted in the current era of CV care may be of greater relevance to current practice. Many of the earlier studies were either conducted in highly selective patient populations, such as the Strong Heart Study in American Indians, or did not include an ABI in defining the presence of PAD. Exclusive reliance for establishing the diagnosis of PAD on the basis of prior cerebrovascular and/or other noncoronary peripheral arterial events or interventions could not only underestimate the prevalence of PAD but also limit the significance of such studies. The findings of our study and that of others on the predictive value of ABI in patients with CAD should be clearly distinguished from those conducted in at-risk patient populations, where there is inadequate evidence that an ABI test result provided additional information to predict CV events, beyond the Framingham risk score [14]. Further, the US Preventive Services Task Force recommendation suggested that research is needed to identify potential high-risk subgroups who might benefit from ABI screening [15].
It is concluded that there is high frequency of CAD in diabetic patients with abnormal ABI. Further studies are needed to determine the risk conferred by this high prevalence of CAD in this age group and steps taken to decrease the associated morbidity and mortality.