Pain in the immediate postoperative period is found to be less after laparoscopic than after conventional surgical techniques. Ropivacaine is often in favour of Bupivacaine to avoid the risks of toxicity. Levo-bupivacaine, a safer version of bupivacaine is a contender to Ropivacaine. We compare the pain relief provided by Ropivacaine and Levo-bupivacaine instilled intra-abdominally during laparoscopic surgery for acute appendicitis.
This is a double blinded randomized placebo- controlled study conducted on 120 patients in a public hospital over a period of 10 months. Using patient control analgesia (PCA), amount of morphine utilized to attain pain scores of 0-1, measured using visual analog score (VAS) was compared among placebo, Ropivacaine and Levo-bupivacanie group.
Data was analysed using analysis of variance with post-hoc multiple comparisons using Bonferroni test and statistical significance was set at p < 0.05. No significant difference was noted between the Ropivacaine and Levo-bupivacaine groups (p = 1); utilization of morphine was similar for both drugs. However, significant difference was noted between placebo and local anaesthetics (p = 0).
There appear to be no difference between Ropivacaine and Levo-bupivacaine in terms of pain relief though Ropivacaine has been indicated to be less potent than Bupivacaine in some studies. Pre-emptive instillation of local anaesthetic for laparoscopic surgery is beneficial for post-operative pain relief.
Abdominal surgeries come with the postoperative problems of pain, nausea, vomiting, chest infections, and risks of DVT, which lead to delayed ambulation, increased morbidity and longer hospital stays, thus increasing health care costs. Laparoscopic surgery has been proven to reduce many of these problems and instillation of local anesthetic to reduce postoperative pain seems to be an added advantage [1-4].
Studies show that overall complications are lesser with laparoscopic surgical procedures [3,5-8]. Since the laparoscopic surgeries are less invasive, most anesthetists in our hospital do not enlist these patients under the acute pain service care. The postoperative pain is usually managed by the surgeons in the ward, often times with paracetamol and oral opioids that then tend to contribute to the increase in incidence of nausea and vomiting. In the recent years, Ropivacaine has been more popularly used because of its safety profile compared to Bupivacaine. Now available is Levobupivacaine which is said to be safer than Bupivacaine and comparable to Ropivacaine in safety profile. Levobupivacaine and Ropivacaine are prepared as the single levorotatory isomer thus have less potential for systemic toxicity [9-12]. There appear to be conflicting results in studies comparing potency of Ropivacaine and Levobupivacaine [12,13]. The aim of this study is to compare the analgesic effect of Ropivacaine and Levo-bupivacaine during the immediate post-operative period (1-6 hours) in patients after laparoscopic appendicectomy.
This study was conducted over a period of 9 months (May 2008 to February 2009) with the help of medical officers of both the anaesthetic and surgical department. It is a double blinded randomized placebo-controlled study. All patients diagnosed as acute appendicitis, who fulfilled the inclusion criteria, were included in the study. The amount of morphine used postoperatively for pain relief using patient controlled analgesia (PCA) was noted during the immediate postoperative period and subsequent 18 hours (Table 1).
Table 1: Inclusion and exclusion criteria for the study. View Table 1
A sample size of 120 was calculated based on a power of 80% and two-sided alpha level at 0.05 to detect a post-operative analgesic consumption of 50%. The dose was calculated based on patients' body weight and the solutions were prepared in a 50-millilitres syringe by the theatre nurse.
Patients were assigned to 3 groups by simple randomization using sealed unlabeled envelopes that contained the name of the solution. The envelopes were opened by the anaesthetist who then prepared the dilution for instillation. In this study the patient and surgeon were blinded. Group A, the placebo group, received 50 mls of 0.9% saline, Group B received 50 mls, (0.75% Ropivacaine plus 0.9% saline) at a dose of 3 mg/kg and Group C received 50 mls, (0.5% Levo-bupivacaine plus 0.9% saline) at a dose of 2 mg/kg. Once under anaesthesia, the surgeon instilled the agent at the intended operative site and the surgery commenced after waiting for 5 minutes.
General anesthesia was employed for all patients to maintain standardization. Patients were given fentanyl and propofol for induction, muscle relaxant, suxamethonium, followed by tracurium, oxygen, nitrous oxide and sevoflurane for maintenance and reversed with atropine and neostigmine combination. They were given only fentanyl intra-operatively and again in the post-operative recovery bay if there was pain.
After the procedure, the patients were observed in the recovery unit for 20 to 30 minutes, ensured were pain free (pain score 0-1) and sent back to the ward where the pain score was monitored. Patient controlled analgesia (PCA) using morphine as the drug of choice was initiated when the scores were 0-1. Patients were advised to use the PCA until they were comfortable and felt that the pain score was 0-1 by their perception.
Side effects of morphine like nausea and vomiting were treated with metoclopramide or promethazine. At the end of 24 hours, the PCA was stopped and the total dose of morphine used was recorded.
This study was approved by the National Medical Research Registry (NMRR), Malaysia (Protocol Number NMRR-08-1134-2289) and the Malaysian research ethical committee. A written consent was obtained from all patients before they were included in this study.
Data were analysed using analysis of variance with post-hoc multiple comparisons using Bonferroni test. Statistical significance was set at p < 0.05. A t-test was also carried out to compare the Ropivacaine and Levo-bupivacanie.
There was a statistical difference between the placebo and local anaesthetic (LA) group in terms of use of PCA morphine (PCAM). P = 0 (Table 2). There was a significantly higher usage of morphine with placebo group (23.03 mg) to attain the required comfortable state than Ropivacaine (11.89 mg) and Levo-bupivacaine group (11.42 mg) (Figure 1 and Table 3).
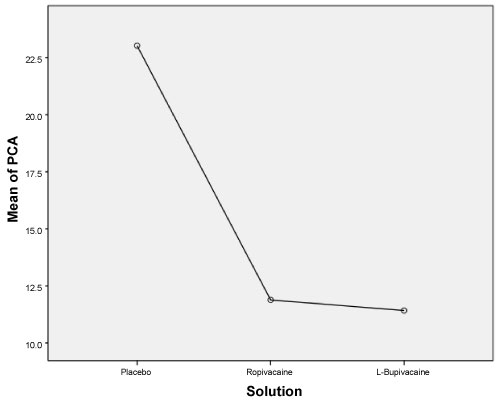 Figure 1: Comparison of placebo, ropivacaine and L. bupivacaine with PCA morphine use. View Figure 1
Figure 1: Comparison of placebo, ropivacaine and L. bupivacaine with PCA morphine use. View Figure 1
Table 2: Relationship of amount of morphine used and the solutions used; A (Placebo), B (ropivacaine) and C (L- bupivacaine). View Table 2
Table 3: Mean dose of morphine used. View Table 3
An independent samples t-test was done also showed no significant difference in the use of morphine for Ropivacaine (M = 11.89, SD = 8.619) and Levo-bupivacaine (M = 11.42, SD = 9.923); t (80) = 0.23, p = 0.821.
There appears to be no correlation between age and amount of PCAM used (Figure 2).
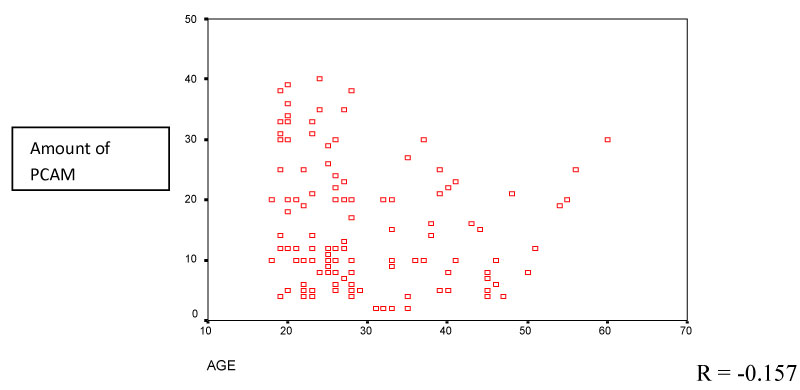 Figure 2: Correlation between age and amount of PCA morphine (PCAM) used. View Figure 2
Figure 2: Correlation between age and amount of PCA morphine (PCAM) used. View Figure 2
Postoperative pain control does influence speedy recovery and discharge of a patient from the hospital and recent studies show that adequate acute pain control would also reduce the risk of developing chronic pain [14,15]. The multimodal analgesic principal is a concept practiced by many anaesthesiologists and surgeons to maximize the analgesic efficacy and minimizing the side-effects associated with the use of each class of analgesics especially opioids. The use of local anesthetics in central and peripheral nerve blockades, which include wound infiltration, can improve pain score in the postoperative period [16].
The reason for replacing racemic Bupivacaine with the s-enantiomers Levo-bupivacaine and Ropivacaine is to provide a wider margin of safety with the same analgesic efficacy and less postoperative motor block. However, on the basis of theory (lower lipophilic property) and many experimental studies, Ropivacaine appears to have the greatest margin of safety of all the local anaesthetics [11,17].
The individual dose of analgesic required for analgesia differs significantly from patient to patient. Pain in fact has an affective and motivational component [18,19]. In our study, there was better pain control in patients who received the local anaesthetic instillation than those who did not, a similar finding with several other studies [1,4,7,20-22]. We found no difference in the pain relief provided by Ropivacaine and Levo-bupivacaine postoperatively. We used the maximum safe dose per kilogram body weight (2 mg/kg for Levobupivacaine and 3 mg/kg for Ropivacaine) for each drug to calculate the total dose for each patient and they were each diluted with 50 milliliters of saline.
Many studies have been done looking at the potency and there appear to be contradictory results depending on the type of anaesthesia the drugs are used for [12,23]. Some studies indicate that for labor analgesia, Ropivacaine and Levo-bupivacaine are equipotent while some found Levo-bupivacaine to be 15% more potent when used in obstetric labor analgesia [24,25]. When used for women in labor, Levo bupivacaine was 19.3% more potent than Ropivacaine (although the difference was not statistically significant) and provided similar safety results [25]. In other studies with similar designs, Ropivacaine was found to be 40% to 50% less potent than Bupivacaine [17,24,25]. There are up-and-down sequential allocation studies in patients receiving epidural analgesia for labor pains that show Levobupivacaine and Bupivacaine to be equipotent as well [26]. A study on obstetric patients receiving spinal anaesthesia Levobupivacaine was found to be 38% less potent than Bupivacaine [27]. However, several studies demonstrate the potency arrangement for spinal and combined spinal-epidural to be Bupivacaine > Levobupivacaine > Ropivacaine [9,11,28].
Factors that need consideration when choosing between drugs with similar clinical profile include safety profile, efficacy and cost. Viewing from an economic perspective, it is difficult to justify the use of Levobupivacaine in place of Ropivacaine when both the drugs have very similar clinical effects especially in terms of safety. The costing of a drug is deciding factor when it comes to purchasing drugs for use in major hospitals and in third world countries Levo-bupivacaine being more expensive than Ropivacaine. It has been established that Levo-bupivacaine and Ropivacaine have similar safety features though there are studies that show that Ropivacaine has slightly less side effects than Levo-bupivacaine. Nonetheless, differences in potencies appear to not affect the efficacy of the drugs as we noted in our study [9].
The average age of patients in our study is 30 years and there appears to be no correlation between age and amount of PCA used in our study.
Pre-emptive instillation of local anaesthetic for laparoscopic surgery is definitely beneficial for post-operative pain relief as very little other analgesic like an opioid maybe needed, allowing patients to ambulate earlier, have less risk of post-operative nausea and vomiting and other ill-effects of morphine/opioids. However, we found no difference the effectiveness of pain relief provided by Ropivacaine and Levo-bupivacaine in our study.