International Journal of Anesthetics and Anesthesiology
Airway Management in a Patient with Metatropic Dysplasia: Grossly Abnormal Anatomy Combined with a Low Functional Residual Capacity
Joseph G. Werner, Alberto A. Uribe*, Karina Castellon-Larios, Sergio D. Bergese and Matthew P. McKiernan
Department of Anesthesiology, Wexner Medical Center, The Ohio State University, USA
*Corresponding author: Alberto Uribe MD, Senior Clinical Research Coordinator, Department of Anesthesiology, Wexner Medical Center, The Ohio State University, 410 W. 10th Avenue N411 Doan Hall, Columbus, OH 43210, USA, Tel: 6143669071, E-mail: alberto.uribe@osumc.edu
Int J Anesthetic Anesthesiol, IJAA-1-007, (Volume 1, Issue 2), Case Report; ISSN: 2377-4630
Received: August 20, 2014 | Accepted: September 22, 2014 | Published: September 29, 2014
Citation:Werner JG, Uribe AA, Larios KC, Bergese SD, McKiernan MP (2014) Airway Management in a Patient with Metatropic Dysplasia: Grossly Abnormal Anatomy Combined with a Low Functional Residual Capacity. Int J Anesthetic Anesthesiol 1:007. 10.23937/2377-4630/1007
Copyright: © 2014 Werner JG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Difficult intubation is a constant concern in surgical and critical care settings due to its direct relationship with morbidity and mortality. The incidence reported in literature varies between 0.1% to 13% and reaches 14% in the obese population [1-4]. The American Society of Anesthesiologists (ASA) defined difficult airway as a situation in which a trained anesthesiologist experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both. They also defined difficult tracheal intubation as an intubation requiring multiple attempts in the presence or absence of tracheal pathology [5]. The complications related to difficult intubation include, but are not limited to: death, hypoxic brain injury, cardiopulmonary arrest, rescue tracheostomy, airway trauma, aspiration, and damage to teeth [1]. Fiber optic intubation and the use of laryngeal mask airways has been a great alternative to manage difficult intubation cases [6]. Different methods and tools have been created and studied to predict a potential difficult intubation case; however, there is not a strong consensus of which one is more used and/or validated.
Metatropic dysplasia is a rare chondrodysplasia characterized by disproportionately short extremities and a long narrow trunk that evolves into a progressive and severe kyphoscoliosis. Facial features include a prominent forehead and squared-off jaw. Other findings may include odontoid hypoplasia, cervical myelopathy, and deafness [7]. The severe kyphoscoliosis and normal adult-sized organs result in restrictive lung disease with poor respiratory mechanics that may warrant tracheostomy and long-term ventilatory support. Laryngotracheomalacia and fused arytenoids, along with redundant pharyngeal tissue, have also been described [8,9].Concerns relating to the airway management of these patients include: atlantoaxial instability, which is almost universally present; restrictive lung disease with low functional residual capacity (FRC) that results in the rapid development of hypoxia; and laryngotracheomalacia with fused arytenoids along with redundant pharyngeal tissue which make direct laryngoscopy challenging.
Case Report
A 24-year-old female with a history of metatropic dysplasia who was admitted to our intensive care unit with hypercapnic (PaCO2 97 mmHg) and hypoxic respiratory failure that had been treated with biphasic positive airway pressure (BiPAP). Recognizing the challenges of airway management in this patient, the critical care team requested that the anesthesiology team be called to perform a fiber optic intubation. On physical exam, the patient was obtunded secondary to her hypercapnea, had a poor oral opening with no participation in airway exam, weighted 39.9 kg and was 41.5 inches tall (BMI 35.5), had a large overriding rib cage with kyphoscoliosis, short limbs, and displayed labored breathing on a BiPAP machine. Her airway exam showed a mallampati class 4 with less than 3 finger breadths oral opening. A chest x-ray showed skeletal dysplasia and some dwarfism (Figure 1A, Figure 1B). Furthermore, a computed tomography pulmonary embolism study revealed a large pericardial effusion and small bilateral pleural effusions, but no evidence of a pulmonary embolism (Figure 1C, Figure 1B) One can observe from these images how the heart and abdominal organs take up a large amount of her thoracic cavity, and when combined with her severe kyphoscoliosis, result in a severe restriction to ventilation.
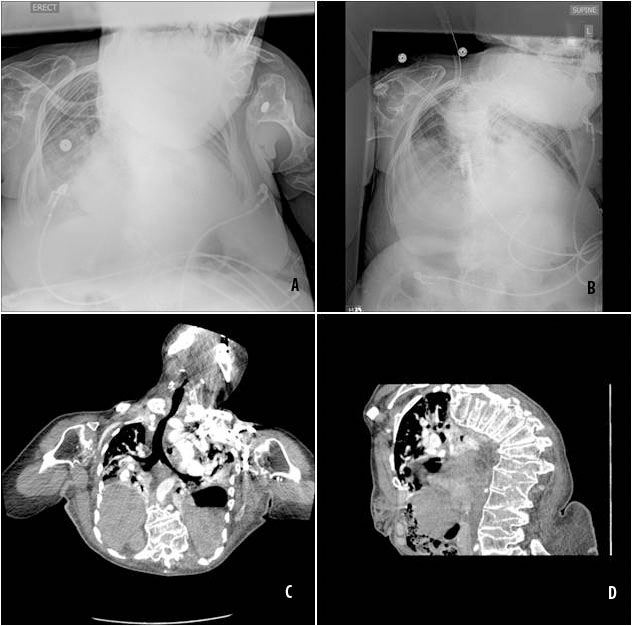
Figure 1: (A-B) Chest x ray upon admission. (C-D) Computed tomography pulmonary embolism study
View Figure 1
It was elected to proceed with fiberoptic intubation with spontaneous ventilation. The patient was obtunded and nonresponsive; her arterial blood gas revealed chronic respiratory acidosis with partial pressure of oxygen 53.20 mmHg, partial pressure of carbon dioxide 109.30 mmHg, pH 7.254, bicarbonate 47.3 mmol/L, oxygen saturation 79.3%, and with a fraction of inspired oxygen (FiO2) of 43%. During preparation of intubation equipment, the patient was pre-oxygenated with 100% oxygen via her BiPAP device, hemodynamically stable (BP 108/52, HR 96, 94% on 100% FiO2). Six attempts with fiber optic intubation failed due to poor visualization of structures combined with a rapidly developing hypoxia (15-20 seconds per attempt) with pulse oximeter readings precipitously dropping in the 40's. As the patient reacted to the airway manipulation, 2 mg of intravenous midazolam was administered. Direct laryngoscopy with MAC 3 and glidescope were also unsuccessful because of the pharyngeal tissue and kyphoscoliosis that made visualization difficult. Assisted bag mask ventilation was done between attempts with pulse oximetry readings in the 92% to 95% range. The use of succinylcholine was contraindicated, as the patient had been bed-ridden for over a month and likely had upregulation of receptors at the neuromuscular junction. Though her spontaneous efforts were insufficient to maintain adequate oxygenation and ventilation, total apnea would have made desaturation occur even faster due to her very small FRC. It seemed unlikely that paralysis would have provided a better view as the pt was very kyphoscoliotic, may have further worsened tissue redundancy as muscle tone relaxed, and movement of the glottis with respiration often helps identify airway structures in patients with challenging anatomy. An i-gel laryngeal mask airway (LMA) #4 was placed without difficulty, and was used to support her spontaneous ventilation. Another fiberoptic intubation was attempted through the LMA with a 6.0 ETT, but was again aborted due to rapid desaturation. Due to her continued rapid desaturation, it became necessary to provide continuous ventilation to the patient while attempting intubation.
A Sontek suction-safe swivel Y bronchoscopic adaptor was placed onto the LMA to offer ventilatory support during intubation attempts and allowed us to manipulate the airway with minimal oxygen desaturation (Figure 2A). The Sontek suction-safe swivel Y bronchoscopic conector is an adaptor created originally to suctioning patient in mechanical ventilators without disconnecting the endotracheal tube from the ventilator and maintaining a positive end expiratory pressure (PEEP) (Figure 2B). It has a self-closing silicone diaphragm through which the bronchoscope is placed, which allowed positive pressure ventilation with minimal leak (Figure 2C). The other advantage of this diaphragm was that it could be cut away to allow the endotracheal tube (ETT) to pass through the adaptor and over the scope using Seldinger's technique (Figure 2D, Figure 2E). This setup was vital in providing adequate oxygen saturation levels, which allowed manipulating the fiberoptic scope in this challenging airway. Despite the i-gel LMA being seated properly, poor visualization of the glottis was present due to redundant pharyngeal tissue. A 6.0 Parker ETT was loaded over the fiberoptic scope, as this size was the largest ETT that could fit through the bronchoscope adaptor, with the diaphragm removed. Even with extreme anteflexion of the scope, her anatomy was grossly abnormal with no recognizable vocal cords, despite spontaneous ventilation. After multiple attempts over 20 minutes by multiple attending anesthesiologists, the tracheal rings were identified while maintaining O2 saturation > 90%. Intubation occurred just before the surgeon was getting ready to prep the neck for a tracheostomy.
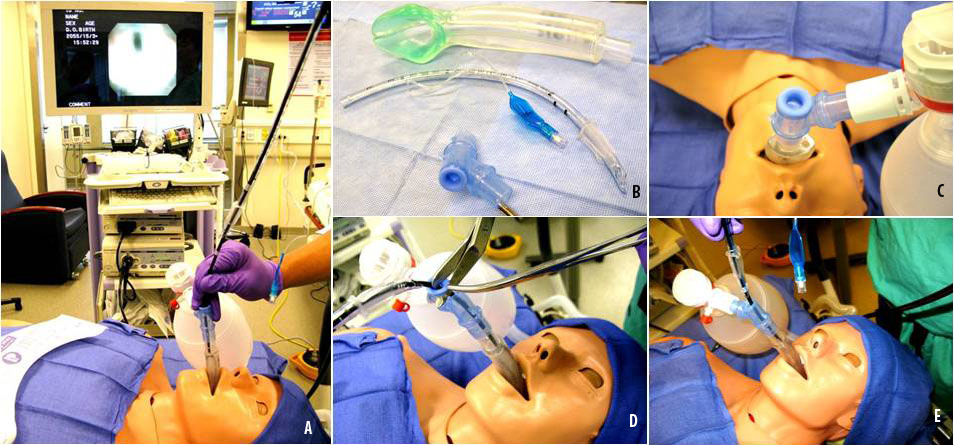
Figure 2: (A) Application of the Sontek suction-safe swivel Y bronchoscopic adapter through the LMA. (B) I-gel laryngeal mask airway (LMA) #4, Endo-tracheal tube and Sontek suction-safe swivel Y bronchoscopic adapter. (C) Diaphragm of the Sontek suction-safe swivel. (D) Diaphragm of the Sontek suction-safe swivel cut. (E) Diaphragm of the Sontek suction-safe swivel removed.
View Figure 2
Discussion
FRC is decreased in patients with restrictive lung disease and carries the risk of rapid desaturation during periods of apnea. If prolonged, this hypoxia puts the patient at risk of hypoxic brain injury, cardiac arrest, or even death. The risk of significant morbidity or mortality is even greater in the setting of a difficult airway. During difficult intubation, the LMA has been proven to be a useful rescue tool, as it allows for the ability to ventilate and serve as a conduit for tracheal intubation. Review of literature found multiple articles that describe its use as a conduit for fiberoptic scope-guided tracheal intubation. One article described the successful use of a bronchoscope adapter swivel elbow piece attached to an LMA during bronchoscope guided intubation in a patient with a difficult airway [10]. In our case, the patient had both a difficult airway and severe restrictive lung disease. The bronchoscope adaptor allowed for continuous ventillatory support during the intubation attempts over a 20-minute time period. In conclusion, when intubating patients with a low FRC, use of an LMA with a bronchial adaptor should be considered as a strategy to intubate the trachea, especially when hypoxia develops rapidly.
Funding Disclosure
Funding provided by the Department of Anesthesiology.
References
-
Yildiz TS, Korkmaz F, Solak M, Toker K, Erciyes N, et al. (2007) Prediction of difficult tracheal intubation in Turkish patients: a multi-center methodological study. Eur J Anaesthesiol 24: 1034-1040.
-
Fox WT, S Harris, NJ Kennedy (2008) Prevalence of difficult intubation in a bariatric population, using the beach chair position. Anaesthesia 63: 1339-1342.
-
Ezri T, Medalion B, Weisenberg M, Szmuk P, Warters RD, et al. (2003) Increased body mass index per se is not a predictor of difficult laryngoscopy. Can J Anaesth 50: 179-183.
-
Enterlein G, C Byhahn (2013) Practice guidelines for management of the difficult airway: update by the American Society of Anesthesiologists task force. Anaesthesist 62: 832-835.
-
Fox GS, DG Whalley, DR Bevan (1981) Anaesthesia for the morbidly obese. Experience with 110 patients. Br J Anaesth 53: 811-816.
-
Zarogoulidis P, Kontakiotis T, Tsakiridis K, Karanikas M, Simoglou C, et al. (2012) Difficult airway and difficult intubation in postintubation tracheal stenosis: a case report and literature review. Ther Clin Risk Manag 8: 279-286.
-
Beck M, Roubicek M, Rogers JG, Naumoff P, Spranger J (1983) Heterogeneity of metatropic dysplasia. Eur J Pediatr 140: 231-237.
-
Genevieve D, Le Merrer M, Feingold J, Munnich A, Maroteaux P, et al. (2008) Revisiting metatropic dysplasia: presentation of a series of 19 novel patients and review of the literature. Am J Med Genet A 146A: 992-996.
-
Kannu P, Aftimos S, Mayne V, Donnan L, Savarirayan R (2007) Metatropic dysplasia: clinical and radiographic findings in 11 patients demonstrating long-term natural history. Am J Med Genet A 143A: 2512-2522.
-
Carron M, U Freo, C Ori (2009) Bronchoscope-guided intubation through a Laryngeal Mask Airway Supreme in a patient with a difficult-to-manage airway. J Anesth 23: 613-615.





