Femoral stem fracture is an extremely rare cause, especially in cementless nonmodular stem femoral. Furthermore, revision surgery for isolated polyethylene wear represents a challenge and dilemma for the orthopedic surgeon. This study aimed to present the first case that described two successive challenging causes of total hip arthroplasty revision, and to detail how they were how they were best managed.
A 65-year-old male patient with a body mass index of 31 who underwent a primary left cementless total hip arthroplasty for the end-stage arthritic hip. 4 years later, he presented a femoral stem fracture diagnosed following the clinical and radiological findings prompting the patient to undergo surgery. Only the femoral component was revised with good results for 5 years. After that, he gradually presented a pain of the left hip with clinical lameness. The radiograph of the hip showed that the femoral head was embedded in the acetabulum component, and so revision surgery was indicated. The intraoperative aspect found a total wearing of the acetabulum's polyethylene then a dual-mobility acetabular component was used while the femoral stem prosthesis was conserved. At a follow-up of 2 years, the patient was pain-free and could ambulate with no assistive devices and no leg length inequality.
However, implant fracture is extremely rare; it can be highly traumatizing for patients. The isolated polyethylene wear remains a serious problem for engineers who manufacture prostheses, for surgeons who implant them and for patients who get the result.
Implant fracture, Polyethylene wear, Revision surgery, Hip prosthesis
Total hip arthroplasty (THA) constitutes currently the cornerstone of surgical management of end-stage arthritic hip conditions [1,2]. The number of patients operated for hip prosthesis has increased substantially over the past several years. At least, this number will be more than 572,000 by the year 2030 [3]. On the other hand, it is known that “the more prosthesis we implant, the more revision surgery, we will perform” that's why, also, the number of revision hip procedures is expected to increase to 96,700 by 2030 [4]. This revision surgery is due to many causes such as periprosthetic fracture, infection, osteolysis. But, implant fracture as one of the modes of failure of total hip arthroplasty is an extremely rare cause, especially in cementless nonmodular stem femoral [5,6]. Moreover, revision surgery for isolated polyethylene wear represents a challenge and dilemma for the orthopedic surgeon [7].
To the best of our knowledge, this is the first such case to be reported in the literature that described two successive challenging causes of total hip arthroplasty revision.
A 65-year-old male patient weighed 94 kg with a body mass index (BMI) of 31, had been diagnosed with osteoarthritis of both hip since 12 years ago; the left side was the more painful (Figure 1A) reason for which he underwent a primary left cementless total hip arthroplasty (Valmer Cup size 50; SILENE femoral stem size 5; ceramic femoral head with long size 28 mm) (Figure 1B)). A Hardinge external approach was performed with neither reported intraoperative nor postoperative complications. The patient did well (no pain of left hip and a tolerated pain of right hip) until 2011 (4 years later) at which time he reported an insidious thigh pain in the left hip, got worse gradually with weight-bearing, unrelieved by medication; his only relief came from rest and restriction of weight-bearing. Two weeks later, when the patient was getting up from a sitting position brutally, he heard a broken sound in his left hip that caused a painful hip movement. Then he was transferred to the emergency department. On Admission, he was in good general health with no distress signs. Physical examination found both palpation and mobilization of the left hip were painful; the homolateral leg was shortened and externally rotated. The neurovascular examination was normal, and the skin of the operative site was good. Emergency radiographs of the pelvis showed a rupture at the neck-stem junction of the femoral component with no associated fracture or bone losing (Figure 2) prompting the patient to undergo surgery. Thus, three days later, after anesthetic preparation, he was admitted to the operating room for revision surgery via the same surgical approach. Intraoperative aspects showed a fracture of the femoral stem; since the extraction of the remainder femoral stem did not seem feasible, we performed a femoral osteotomy; it was removed after making it free; the acetabulum was well fixed with no evidence of scratches or loosening and so the cup was not revised. A multiple stainless steel cerclage wires were inserted to secure extended trochanteric osteotomy (Figure 3): Implanted components included a femoral revision stem cemented size 4 and 28 mm ceramic femoral head with a medium neck. Hip exercises such as touching the floor without weight-bearing and transfer onto a wheelchair were permitted 3 weeks postoperatively; partial weight-bearing was permitted at 8 weeks postoperatively, and complete weight bearing with support from a T-cane was allowed 3 months postoperatively. Six months later, the patient regained his usual activities with a good Postel-Merle-d'Aubigne function score.
 Figure 1: A) Anterior-posterior pelvic x-ray showed advanced left hip osteoarthritis (Femoral offset = 41 mm); B) On post-operative x-ray control, Femoral offset = 38 mm, cap inclination = 33°. View Figure 1
Figure 1: A) Anterior-posterior pelvic x-ray showed advanced left hip osteoarthritis (Femoral offset = 41 mm); B) On post-operative x-ray control, Femoral offset = 38 mm, cap inclination = 33°. View Figure 1
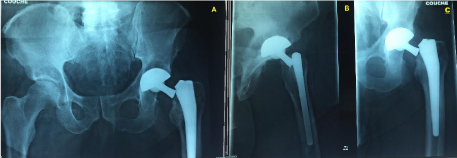 Figure 2: Emergency radiographs (anterior-posterior views of the pelvis (A), of the hip (C) and lateral view of the hip (B) showed a rupture at the neck-stem junction of the cementless nonmodular stem femoral with neither associated fracture nor bone losing. View Figure 2
Figure 2: Emergency radiographs (anterior-posterior views of the pelvis (A), of the hip (C) and lateral view of the hip (B) showed a rupture at the neck-stem junction of the cementless nonmodular stem femoral with neither associated fracture nor bone losing. View Figure 2
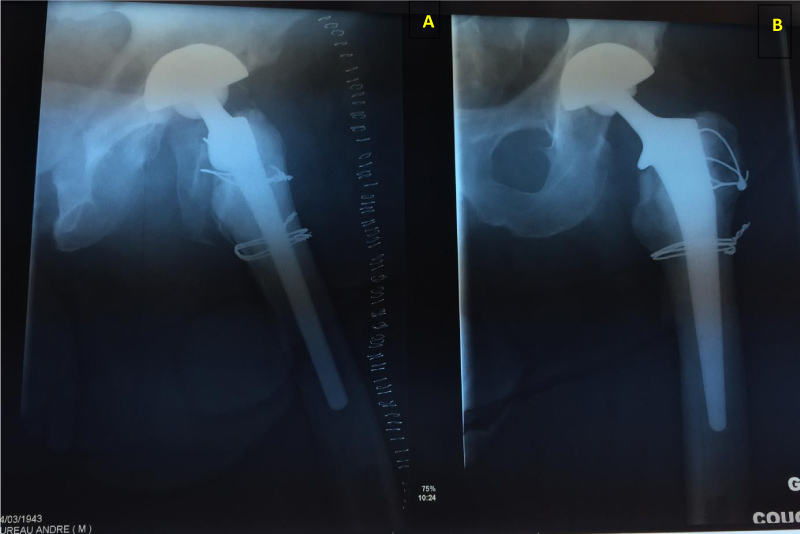 Figure 3: The post-operative X-rays of the left hip ( lateral (A) and anterior-posterior (B) views ) showed a good fixation of the components.
View Figure 3
Figure 3: The post-operative X-rays of the left hip ( lateral (A) and anterior-posterior (B) views ) showed a good fixation of the components.
View Figure 3
The patient remained asymptomatic until 5 years when he reported an insidious onset of the progressive left hip pain that is relieved partially with analgesic oral. The evolution was marked by the appearance of clinical lameness requiring the use of crutches that forced the patient to get a visit to our department. At this follow up, with a body mass index of 36, he reported that his limb has been getting shorter. Physical examination found a shortened left lower extremity of 2 cm; the X-ray of the pelvis showed that the femoral head was embedded in the acetabulum component (Figure 4A). Erythrocyte sedimentation rate and C-reactive protein values were normal. The surgical treatment was established. A few days later, the patient was taken to the operating room; under general anesthetics, an incision was made through the previous scar followed by an appropriate dissection, after which, the Intraoperative aspects showed that the femoral head was slightly damaged and the acetabulum's polyethylene was totally worn; the femoral component was in excellent condition. Implanted components included a dual-mobility acetabular component cemented size 54 and ceramic femoral head with medium neck size 28 mm (Figure 4B). The patient's initial postoperative course was uncomplicated. At a follow-up of 2 years, the patient was pain-free and could ambulate with no assistive devices and no leg length inequality.
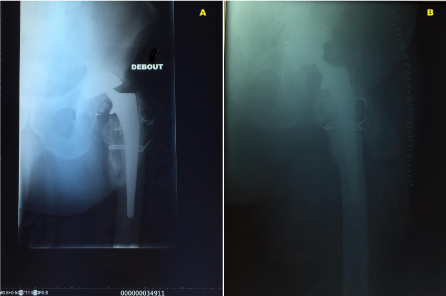 Figure 4: A) The anterior-posterior hip radiograph revealed a protrusion of the prosthetic femoral head through the acetabulum component (fracture of the head femoral or damaged of the polyethylene were suspected); B) postoperative radiograph control showed the normal position of the acetabulum component.
View Figure 4
Figure 4: A) The anterior-posterior hip radiograph revealed a protrusion of the prosthetic femoral head through the acetabulum component (fracture of the head femoral or damaged of the polyethylene were suspected); B) postoperative radiograph control showed the normal position of the acetabulum component.
View Figure 4
The numbers of revisions of both primary and revision hip implantations are steadily increasing [8]. Revision implantation is more challenging than a primary procedure as the bone stock has often been lost due to stress shielding and the operative removal of the primary implant and the cement mantle, mostly in the proximal region. Many causes of revision surgery are well identified and documented and are regularly studied in the literature [9]. Implant fractures after total hip arthroplasty (THA) are relevant complications for patients, physicians, and the public health system leading to high socioeconomic burdens [10]. When an implant fracture occurred, it is generally an unacceptable complication for the patient and it is not reconcilable with a satisfactory outcome [11]. These fractures occurred between 14 months and 5 years, postoperatively [12]. Reports in the literature have identified multiple risk factors for revision surgery due to prosthetic stem fracture, including higher levels of activity, relatively younger age, male gender, valgus stem positioning, and relatively undersized stem relative to the patient's anatomy, increased femoral head size, increased femoral offset, and increasing patient weight [13-15]. Currently, Obesity is undeniably a risk factor for poor outcomes and complications after total hip replacement including implant fracture. Almost all cases of implant fractures described in the literature occurred in patients with high BMI [6,16] as in our case.
On the other hand, in revision surgery, the instability of a total hip prosthesis is due to many factors such as age, BMI, ossification, extended liberation of soft tissue, surgical approach and polyethylene wear [17,18]. The conventional polyethylene linear and volumetric wear is increased when the acetabular inclination is greater than 45° [19]. Furthermore, when a diagnosis of isolated polyethylene wear is established, the surgeon must decide whether to exchange the polyethylene alone or revise the acetabular cup instead, especially when he encountered a well-fixed acetabular component. In fact, some authors recommend the complete acetabular revision because the exchange of polyethylene alone increases significantly the risk of instability and dislocation [20] whereas other authors support the exchange of polyethylene alone because of the low dislocation rates in their series and considering that the acetabular revision may cause significant bones losing especially for well-fixed acetabular components [21]. So relying on those factors, there is a question that remains to be answered: Should we have revised the conventional cup, during the first surgery revision, although it was acceptably oriented and well-fixed with no macroscopic wear of the acetabulum's polyethylene? Could this management avoid the second complication? It is still controversial [17].
Although, the dual mobility cup has the great merit to considerably reduce the risk of dislocation rate, and to resist to polyethylene wear in revision surgery, we did not prefer to revise the acetabulum because there was no macroscopic polyethylene wear and the acetabulum was acceptably oriented and well-fixed and so its extraction, re-implantation would be challenging, and it could cause bone loosening that may be difficult to restore.
At last, we emphasize that the experimental study or metallurgical analysis of the broken implant and computed tomography would be helpful to understand well, the exact cause of failure of the primary hip prosthesis. However, we think that the real cause of implant fracture was most probably multifactorial including high BMI, corrosion fatigue of the femoral stem and excessive solicitation of the prosthesis. On the other hand, the revision surgery, high BMI and the inclination of the acetabular less than 35° were probably the main causes of the acetabulum's polyethylene wear.
In conclusion, although it is an extremely rare event, implant fracture can be highly traumatizing for patients. The isolated polyethylene wear remains a serious problem for engineers who manufacture prostheses, for surgeons who implant them and for patients who get the result. Finally, we believe that the combination of physical configuration and design of the implant components preoperative risk assessment, optimal surgical technique, and an adequately experienced orthopedic surgeon may promote a good outcome.
The authors declare no conflict of interest.
Nil.
Nil.
All authors contribute to the work.