Cardiac lipoma is a very rare primary benign tumor, with approximately 60 cases reported in the literature [1], with only six cases of lipoma originating from the interventricular septum [2]. It also affects genders and ages.
It is considered as a encapsulated neoplasm composed of mature fat cells and differentiated from the lipomatous hypertrophy of the septum in which there is a deposition of unencapsulated fat. Lipoma can occur anywhere in the heart, while lipomatous hypertrophy is limited to the septum [3].
The present article reports the case of a 24-year-old woman who obtained this diagnosis after the manifestation of degenerated ventricular tachycardia for ventricular fibrillation.
A 24-year-old female patient was admitted to the emergency room with palpitations associated with precordial pain and dyspnea. She was pale, sweating, with the heart rate 220 bpm and blood pressure 80 × 40 mmHg. The ECG demonstrated a sustained ventricular tachycardia rhythm evolving to a ventricular fibrillation rhythm. Four defibrillation attempts were performed with 360 J until obtained to sinus rhythm. Initiated amiodarone infusion, and remained with hemodynamic parameters stable.
Due to investigation, the patient presented with a simple x-ray of the chest (Figure 1) an increase of the cardiac area in posterolateral projection. An echocardiogram showed measurements of normal cardiac chambers, walls and ventricular function. An extrahepatic, homogeneous structure was identified, with minimum measurements of 13 × 13 mm, with infiltration of the interventricular septum, adhered to the pericardium, with increased refraction leading to cardiac displacement (Figure 2).
 Figure 1: X-ray of the chest.
View Figure 1
Figure 1: X-ray of the chest.
View Figure 1
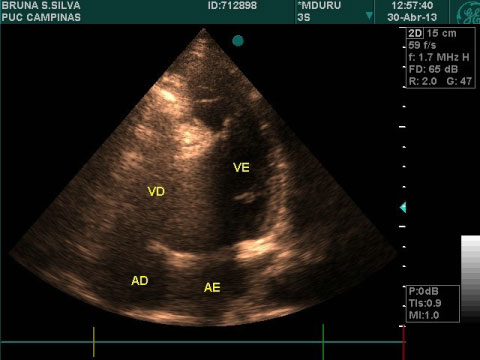 Figure 2: An echocardiogram showed measurements of normal cardiac chambers, walls and ventricular function.
View Figure 2
Figure 2: An echocardiogram showed measurements of normal cardiac chambers, walls and ventricular function.
View Figure 2
It presented hypersignal in the Double IR sequence (similar to fat) without evidence of late enhancement, suggesting lipoma with septal invasion (Figure 3).
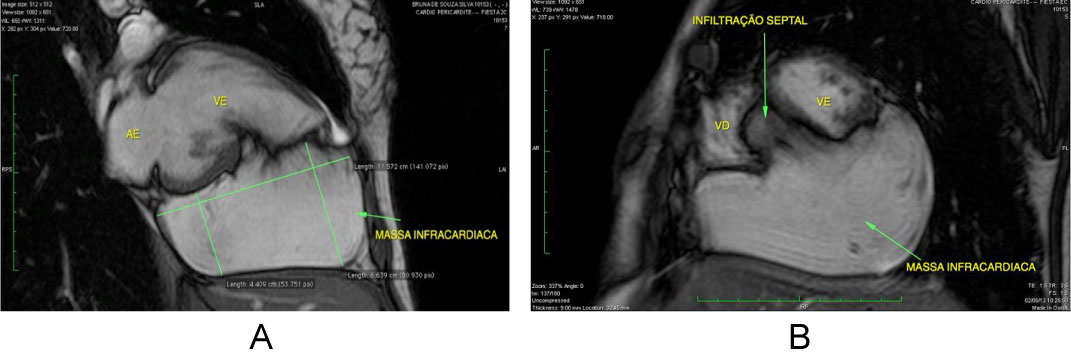 Figure 3: Hypersignal in the Double IR sequence.
View Figure 3
Figure 3: Hypersignal in the Double IR sequence.
View Figure 3
Cardiac surgery was performed with left inframammary thoracotomy, with extracorporeal circulation, and mass excision of adipose tissue, encapsulated in its greatest extent, measuring 13 × 13 × 3.8 cm and 365 g weight (Figure 4). There is not a cleavage plane in the interventricular septum.
 Figure 4: Mass excision of adipose tissue.
View Figure 4
Figure 4: Mass excision of adipose tissue.
View Figure 4
Pathological anatomy (Figure 5) and immunohistochemistry (Figure 6) confirmed the lipoma hypothesis.
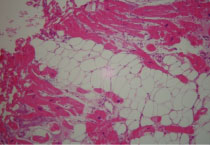 Figure 5: Pathological anatomy.
View Figure 5
Figure 5: Pathological anatomy.
View Figure 5
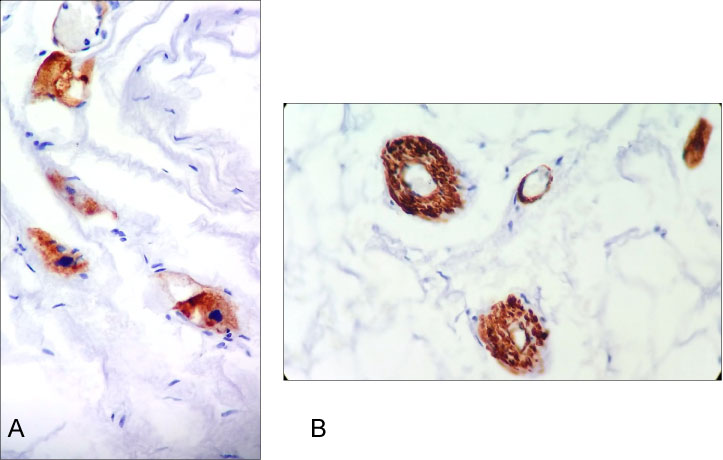 Figure 6: Immunohistochemistry confirmed the lipoma hypothesis.
View Figure 6
Figure 6: Immunohistochemistry confirmed the lipoma hypothesis.
View Figure 6
In the postoperative period, it evolved without intercurrences. In the seventh postoperative period, a new cardiac resonance was demonstrated that showed a moderate amount of lipomatous tissue infiltrating the basal septal region. Decided by the implantation of cardio-defibrillator given the potential risk of new arrhythmias. He returned after 6 months, asymptomatic, with no evidence of an arrhythmogenic event.
She remained in an outpatient clinic, asymptomatic, without arrhythmogenic events. After 3 years of follow-up, the patient was admitted to emergency room, with lipothymia. An ECG was performed and sustained ventricular tachycardia was verified and then she was submitted to electrical cardioversion. In the evaluation of the CDI, it was verified 6 episodes of cardioversion by the device.
New examinations were performed and, due to the impossibility of performing cardiac resonance, using an implantable cardioverter defibrillator, PetCT was chosen (Figure 5) for mass measurement and evaluation of tumor characteristics, considering the evolution of the condition.
Due to infiltration of the lipoma, an extensive area affected and electrical instability, cardiac transplantation was chosen after discussion in Heart Team. It entered as a priority in the heart transplant queue, having performed the procedure as definitive treatment.
The authors emphasize the importance of lipoma as a differential diagnosis of cardiac arrest. Although they are rare, they can leads to complex ventricular arrhythmias and sudden death, successfully reversed in the present case.